Tier 2 Drugs: What They Are, Why They Matter, and How to Use Them Safely
When your insurance plan lists medications in tiers, Tier 2 drugs, prescription medications that cost more than basic generics but less than brand-name or specialty drugs. Also known as preferred brand drugs, they sit in the middle of your formulary—offering a balance between cost and coverage. These aren’t the cheapest pills on the list, but they’re often the most practical choice for long-term treatment. If you’ve ever wondered why your copay for a certain pill is $25 instead of $10 or $50, it’s because of this tier system.
Tier 2 drugs include many commonly prescribed medications like cyclosporine, an immunosuppressant used after organ transplants, terazosin, a blood pressure medication that can cause dangerous spikes if stopped suddenly, and sevelamer, a phosphate binder for kidney patients. These aren’t obscure drugs—they’re daily essentials for thousands. But because they’re not first-line generics, insurers often require prior authorization or step therapy before approving them. That means you might have to try a cheaper Tier 1 option first, even if your doctor knows Tier 2 works better for you.
Why does this matter? Because the difference between Tier 1 and Tier 2 can mean hundreds of dollars a year. A study from the American Journal of Managed Care found that patients switching from Tier 2 to Tier 1 drugs saved an average of $420 annually—but sometimes at the cost of effectiveness. For example, switching from one brand of Tier 2 drugs like tacrolimus to a generic version can trigger rejection in transplant patients due to tiny differences in absorption. That’s why knowing your drug’s tier isn’t just about price—it’s about safety. And if you’re on a medication like dapoxetine or valproic acid, which have narrow therapeutic windows, getting the right version matters just as much as taking it on time.
Insurance plans use Tier 2 to control costs without fully cutting off access. But the system isn’t perfect. Some patients get stuck paying more because their doctor didn’t know a cheaper alternative exists, or because the pharmacy switched their prescription without telling them. That’s why reading your medication label, understanding your formulary, and asking your pharmacist about alternatives is so important. You don’t need to be a medical expert—you just need to know enough to ask the right questions.
Below, you’ll find real-world guides on how to handle these drugs safely: from storing high-risk medications to spotting overdose signs, comparing generics, and avoiding dangerous interactions. Whether you’re managing hypertension, kidney disease, or mental health, the posts here give you the tools to navigate Tier 2 drugs without guessing—or overpaying.
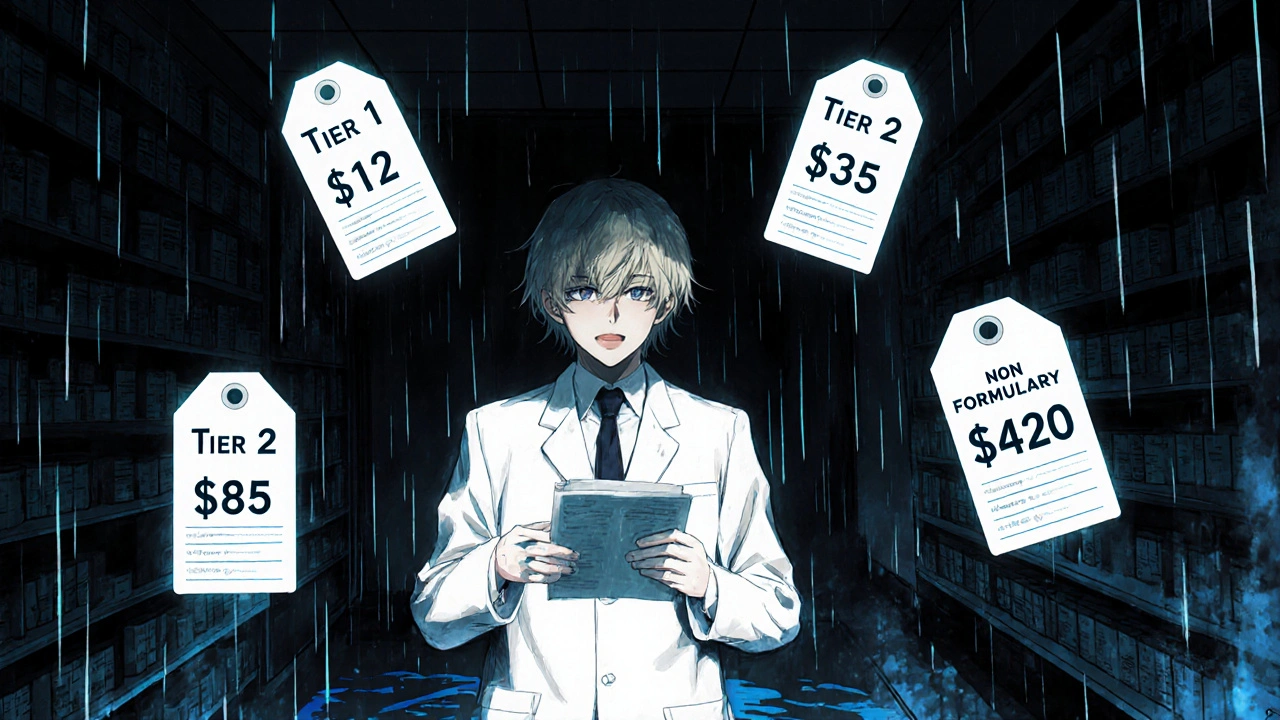
Insurance Formulary Tiers Explained: Tier 1, Tier 2, Tier 3, and Non-Formulary Drugs
Nov, 16 2025
