Tier 1 Drugs: What They Are, Why They Matter, and How to Use Them Safely
When you pick up a prescription, the price you pay often depends on something called a Tier 1 drug, a medication placed in the lowest cost category by insurance plans because it’s proven effective, widely available, and often generic. Also known as preferred generic, it’s the first option your plan encourages because it saves money without sacrificing safety or results. These aren’t just cheap pills—they’re the backbone of affordable healthcare. If you’re on Medicare, Medicaid, or private insurance, you’ve likely taken a Tier 1 drug without even realizing it. Think of common meds like lisinopril for blood pressure, metformin for diabetes, or atorvastatin for cholesterol. These are the drugs your doctor reaches for first because they work, they’re safe, and your insurance wants you to use them.
Tier 1 drugs are chosen through a careful process. Pharmacy benefit managers (PBMs) and insurance companies review clinical data, cost, and real-world use before placing a drug in Tier 1. They look for generics that match brand-name effectiveness, drugs with high patient adherence rates, and those with low risk of serious side effects. This isn’t random—it’s science-backed cost control. A Tier 1 drug might cost you $5 or less per month, while a Tier 3 or 4 drug could run $50 or more. That difference adds up fast, especially if you take meds long-term. But here’s the catch: not all generics are equal. For drugs with a narrow therapeutic index—like cyclosporine, an immunosuppressant used after organ transplants—switching brands can be risky. Even small changes in absorption can lead to rejection or toxicity. That’s why some doctors stick to brand names for these, even if they’re not Tier 1.
Tier 1 drugs aren’t just about price. They’re tied to how you manage your health. If you’re on blood pressure meds, your doctor might start you on a Tier 1 like hydrochlorothiazide before trying anything else. If you have acid reflux, omeprazole is likely your first option. These choices aren’t arbitrary—they’re based on decades of evidence. But knowing your plan’s formulary matters. Just because a drug is Tier 1 doesn’t mean it’s right for you. Some people react poorly to certain generics. Others need a specific formulation. That’s why understanding your medication labels, checking for dosing errors, and tracking side effects (like with valproic acid, a mood stabilizer that can affect energy and appetite) is just as important as knowing the tier.
And it’s not just about taking pills. How you store them matters too. High-risk meds like opioids or sedatives need secure storage, even if they’re Tier 1. Accidental overdoses happen when people don’t realize how dangerous these common drugs can be. Same with withdrawal—stopping something like terazosin, an alpha blocker used for blood pressure and prostate issues suddenly can spike your blood pressure. Tier 1 doesn’t mean risk-free. It means cost-effective. You still need to know how it works, how to take it, and what to watch for.
Below, you’ll find real-world guides on how these drugs behave, how to spot problems, and how to compare alternatives when your plan doesn’t cover what you need. Whether you’re managing chronic illness, dealing with side effects, or trying to save money without sacrificing care, these posts give you the facts—not the fluff.
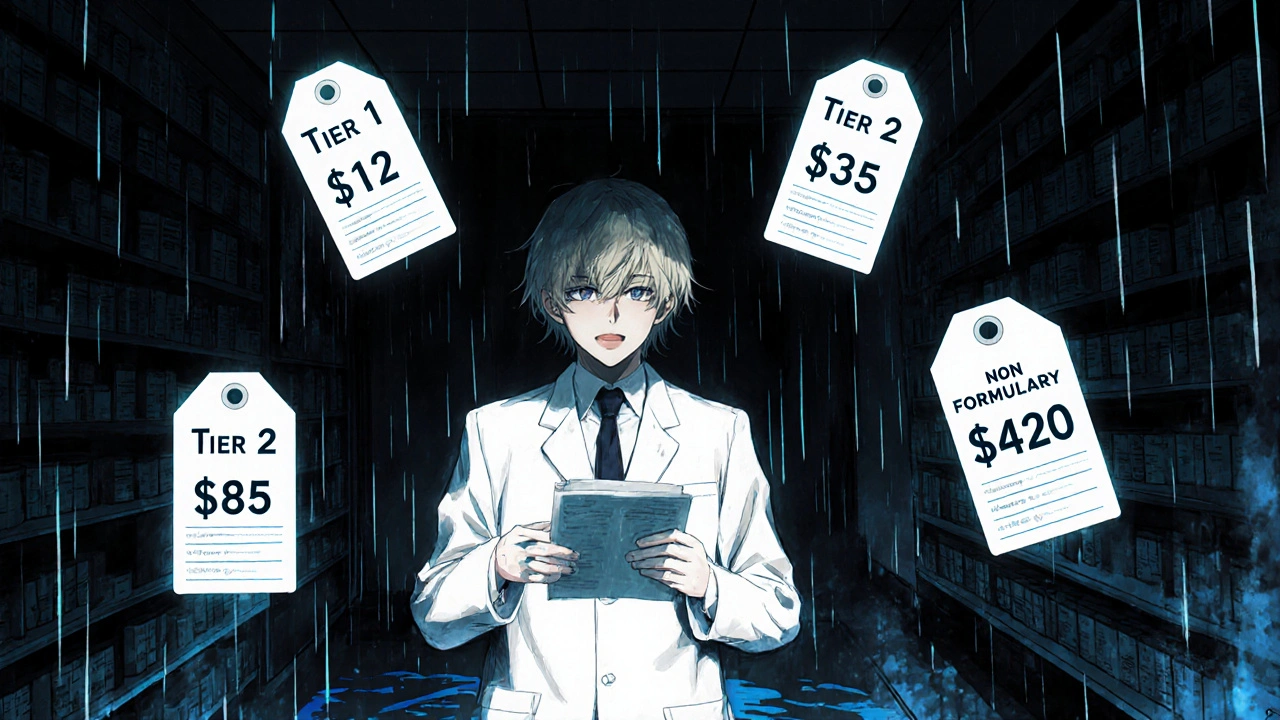
Insurance Formulary Tiers Explained: Tier 1, Tier 2, Tier 3, and Non-Formulary Drugs
Nov, 16 2025
