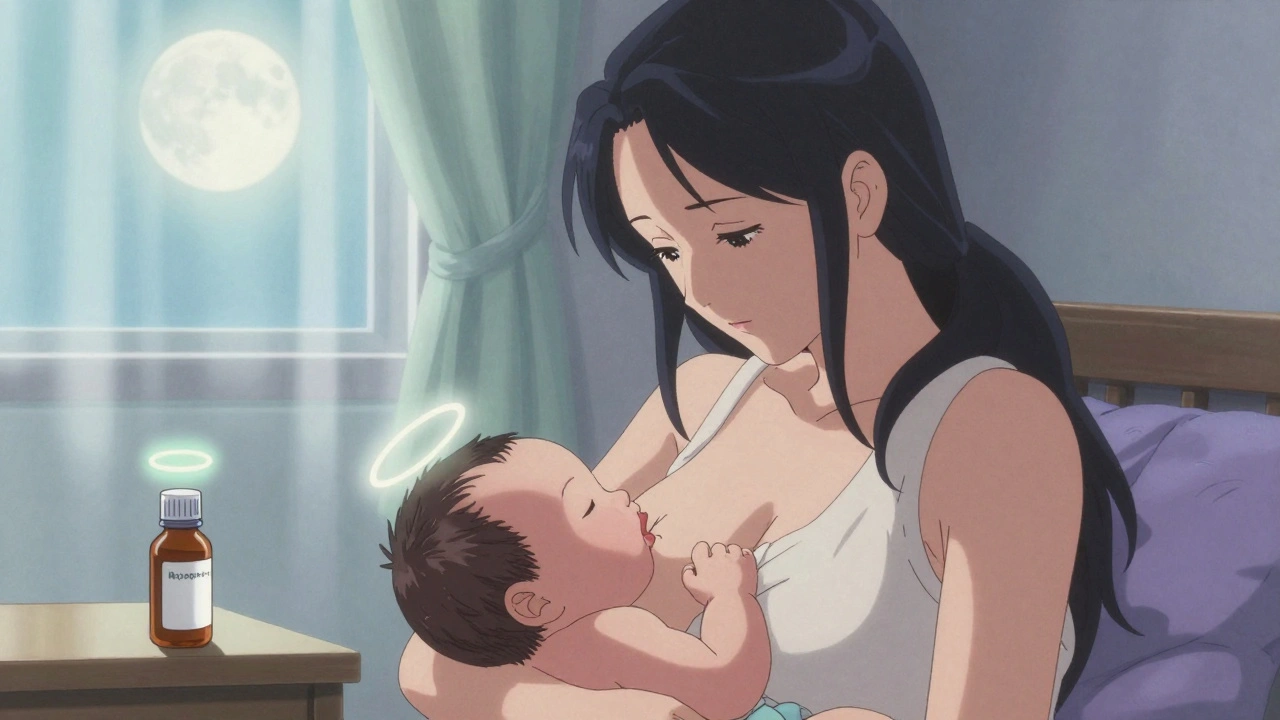
Breastfeeding Pain Meds: Safe Options and What to Avoid
When you're nursing and in pain, the last thing you want is to choose between feeling better and keeping your baby safe. Breastfeeding pain meds, medications used to manage discomfort while nursing, including common over-the-counter and prescription options that pass into breast milk in small amounts. Also known as lactation-safe analgesics, these are not one-size-fits-all—what works for one person might not be right for another, especially when your baby is newborn or premature. The good news? Many pain relievers are considered safe when used correctly, but you need to know which ones to pick and how to use them.
Not all pain meds are created equal when it comes to breastfeeding. Acetaminophen, a common pain reliever and fever reducer often recommended as first-line for nursing mothers. Also known as paracetamol, it enters breast milk in tiny amounts and rarely causes issues, even with regular use. Same goes for ibuprofen, an NSAID that’s broken down quickly in the body and shows up in breast milk in minimal, harmless levels. Also known as Motrin or Advil, it’s often preferred over other anti-inflammatories because it clears out fast and doesn’t build up in your baby’s system. On the flip side, some medications like codeine or certain migraine drugs can be risky—your body might turn them into stronger compounds that your baby can’t process safely. Even something as simple as a cold medicine can hide dangerous ingredients like pseudoephedrine, which can dry up your milk supply.
It’s not just about the drug itself—it’s about timing, dose, and your baby’s age. A single dose of ibuprofen after a dental procedure? Usually fine. Daily use of a stronger painkiller for weeks? That’s when you need to talk to your doctor. Babies under six weeks are especially sensitive because their livers and kidneys aren’t fully developed. And if your baby was born early or has health issues, even safe meds might need extra caution. Always check with your provider before starting anything new, even if it’s sold over the counter.
There’s also more to pain than pills. Breastfeeding pain often comes from latch issues, engorgement, or mastitis—not just general aches. Fixing the root cause can mean less need for meds altogether. A lactation consultant can help with positioning, pumping routines, or warm compresses that reduce swelling and discomfort without touching a single tablet. Sometimes, the best pain relief isn’t chemical at all.
Below, you’ll find real-world advice from people who’ve been there—what worked, what didn’t, and what to watch out for when managing pain while feeding your baby. No fluff, no guesswork. Just clear, practical info to help you feel better without risking your little one’s health.
How to Manage Postpartum Pain Medications While Breastfeeding Safely
Dec, 1 2025
