Managing Postpartum Pain Without Stopping Breastfeeding
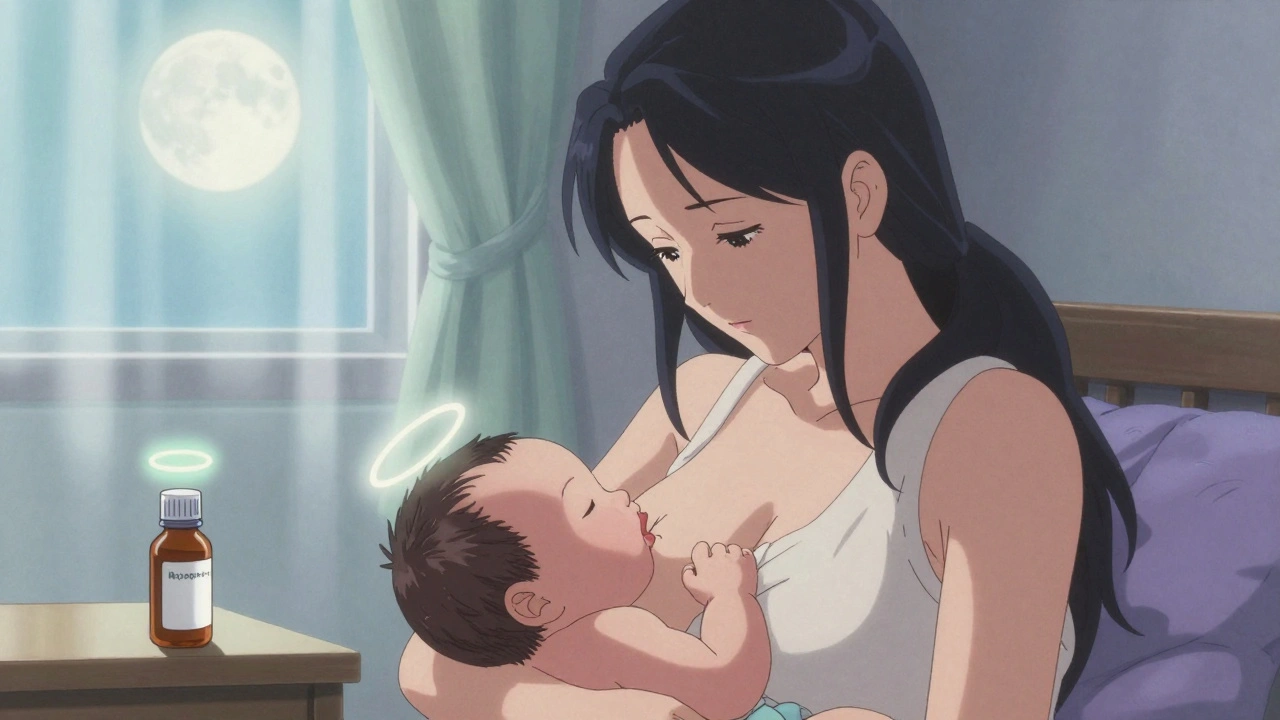
You just gave birth. Your body is healing-whether you had a vaginal delivery or a C-section-and the pain is real. But you also want to breastfeed. You’ve heard conflicting advice: avoid all meds, pump and dump, or worse, stop breastfeeding. None of that is necessary. Most pain medications are safe while breastfeeding, but not all. The key isn’t avoiding medicine-it’s choosing the right ones and using them correctly.
First-Line Choices: Acetaminophen and Ibuprofen
When it comes to postpartum pain, acetaminophen (Tylenol) and ibuprofen (Advil, Motrin) are your safest, most effective options. These aren’t just "probably safe"-they’re backed by decades of research and recommended by the American College of Obstetricians and Gynecologists (ACOG), the Academy of Breastfeeding Medicine, and the FDA.
Acetaminophen passes into breast milk at just 0.1-1.0% of your dose. Ibuprofen is even lower-only about 0.6-0.7%. Neither affects your baby’s sleep, feeding, or development. In fact, studies show infants get less medication from breast milk than they would from a single drop of liquid medicine.
Use them together. Alternating doses every 3 hours gives you steady pain control without overloading your system. For example: take acetaminophen at 8 a.m., ibuprofen at 11 a.m., acetaminophen at 2 p.m., and so on. This keeps your pain managed while keeping your baby’s exposure minimal.
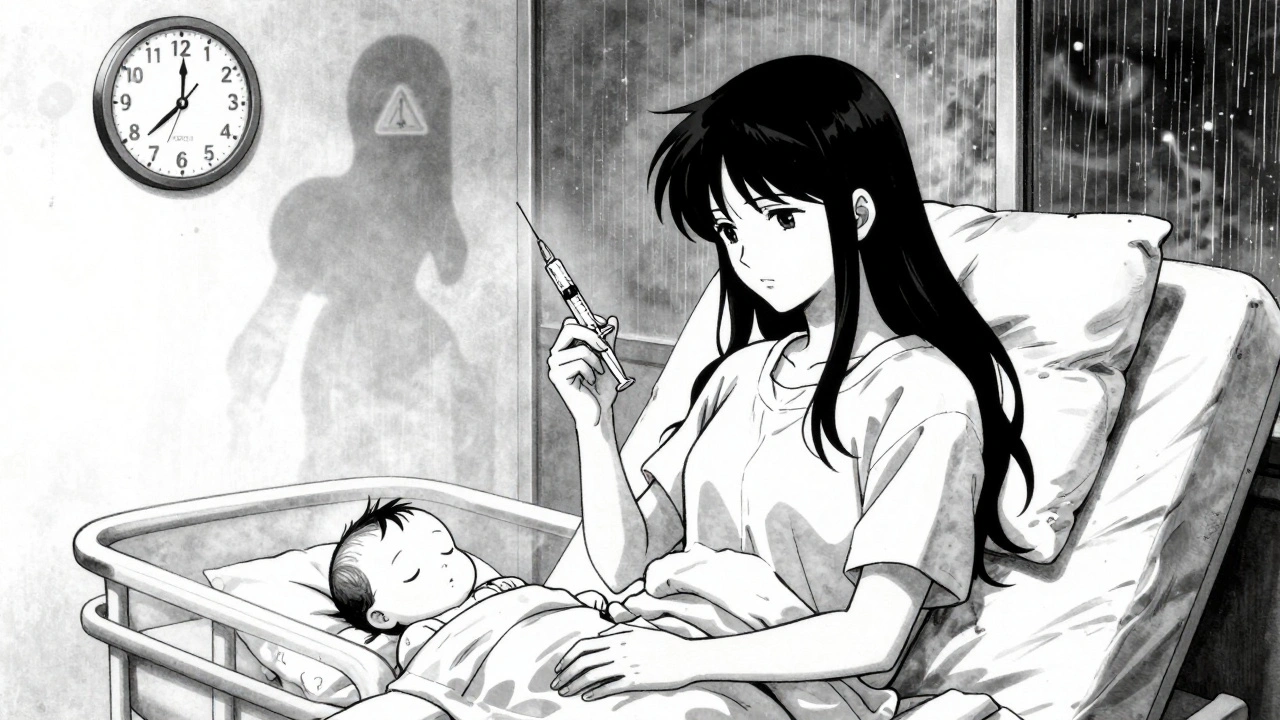
Why Codeine and Tramadol Are Dangerous
Some doctors still prescribe codeine or tramadol for postpartum pain. Don’t take them. The FDA issued strong warnings in 2017 and 2018 because these drugs can turn deadly for breastfed babies.
Here’s why: your body breaks down codeine into morphine, and tramadol into an active metabolite called M1. But not everyone processes them the same way. About 1 in 100 white women are "ultra-rapid metabolizers"-their bodies convert these drugs into morphine or M1 way too fast. That means your breast milk can suddenly contain 10 to 20 times more morphine than normal.
Infants exposed to high morphine levels become dangerously sleepy, have trouble latching, or stop breathing. There have been multiple infant deaths linked to these drugs in breastfeeding mothers. The FDA says breastfeeding is "not recommended" while taking codeine or tramadol. Even one accidental dose can be risky. If you’ve already taken it, watch your baby closely for 24 hours for signs like extreme drowsiness, limpness, or shallow breathing. Call your pediatrician immediately if you see any.
When Opioids Are Necessary: Morphine Is the Safest
If your pain is too severe for acetaminophen and ibuprofen alone-say, after a C-section-you might need an opioid. But not all opioids are equal.
Morphine is the preferred choice. Why? Because babies absorb less than 1% of the morphine that enters breast milk. It’s poorly absorbed in their gut, so even if it’s there, it doesn’t reach their bloodstream in meaningful amounts. Studies show morphine has a relative infant dose (RID) of 8-10%, which is considered low-risk.
Oxycodone is sometimes used too, but it transfers at slightly higher levels (0.1-0.5% of your dose) and can cause drowsiness in babies. Fentanyl and hydromorphone are also options, but only for short-term use.
Never use hydrocodone, codeine, or tramadol. They’re unpredictable. Morphine is the only opioid with consistent, well-understood behavior in breastfeeding.
How to Time Your Doses for Maximum Safety
Timing matters. If you’re taking an opioid, don’t take it right before feeding. Take it right after you breastfeed. That gives your body time to process the drug before the next feeding.
Peak levels in breast milk happen 1-2 hours after you take the medication. So if you take morphine at 7 p.m., wait until 9 or 10 p.m. to feed again. That way, your baby gets the lowest possible dose.
For non-opioids like acetaminophen and ibuprofen, timing doesn’t matter. You can take them whenever you need them-even right before feeding. They’re safe at any time.
What to Avoid: Naproxen, Indomethacin, and Long-Term Use
Some NSAIDs like naproxen (Aleve) and indomethacin are not recommended for breastfeeding mothers, especially in the first few weeks. These drugs stay in your system longer and can build up in breast milk. Naproxen reaches 1.5-2.0% of your dose in milk after 24 hours, which is high enough to potentially cause side effects in newborns or premature babies.
Even ibuprofen should be limited if you’re feeding a preemie or a baby under 2 months old. Stick to the lowest effective dose for the shortest time possible.
Long-term opioid use (beyond 4-6 days) increases the risk of dependency and infant sedation. If your pain lasts longer than a week, talk to your doctor about non-medication options like physical therapy, ice packs, or pelvic floor exercises.
Monitoring Your Baby for Warning Signs
Even with safe medications, watch your baby closely. Signs of opioid sedation include:
- Excessive sleepiness (hard to wake for feeds)
- Lethargy or limpness
- Difficulty latching or sucking
- Shallow or irregular breathing
- Constipation or reduced stooling
If you notice any of these after taking an opioid, stop the medication and contact your pediatrician right away. These signs can appear hours after a dose, so monitor for at least 24 hours.
With acetaminophen and ibuprofen, you don’t need to monitor. Babies tolerate them without issue. No need to wake them for feeds or check for side effects.

What About Anesthesia After Delivery?
You don’t need to "pump and dump" after anesthesia. That old advice is outdated. The Academy of Breastfeeding Medicine updated its guidelines in 2021 after reviewing 15 years of data. Most anesthetics leave your system within hours, and the tiny amounts in breast milk don’t affect your baby.
Wake up, hold your baby, and start breastfeeding. It’s safe. In fact, early breastfeeding helps your recovery and reduces your need for pain meds later.
Future Options: Genetic Testing and Personalized Care
Right now, there’s no routine test to see if you’re an ultra-rapid metabolizer. But researchers at Mayo Clinic are studying CYP2D6 genetic testing to identify women at risk before prescribing codeine or tramadol. It’s not standard yet-but in the future, a simple saliva test could prevent tragedies.
Until then, the safest rule is simple: avoid codeine and tramadol completely. Stick to acetaminophen and ibuprofen. Use morphine only if absolutely necessary, and always time it right.
Bottom Line: You Can Heal and Breastfeed
Postpartum pain doesn’t mean you have to choose between comfort and breastfeeding. You can do both. Start with acetaminophen and ibuprofen. Avoid codeine and tramadol at all costs. If you need something stronger, morphine is your safest bet. Time your doses wisely. Watch your baby. And know that you’re not alone-millions of mothers manage postpartum pain safely every year while breastfeeding.
Trust the science. Not the myths. Your body knows what to do. Your baby needs you. And with the right meds, you can do both-without risk.
Can I take ibuprofen while breastfeeding?
Yes. Ibuprofen is one of the safest pain relievers for breastfeeding mothers. Only 0.6-0.7% of your dose passes into breast milk, and it doesn’t affect your baby’s feeding, sleep, or development. You can take it at any time, even right before breastfeeding.
Is acetaminophen safe for breastfeeding mothers?
Yes. Acetaminophen is considered safe and is often the first choice for postpartum pain. Only 0.1-1.0% of your dose enters breast milk. It’s well-studied, doesn’t cause drowsiness in babies, and can be taken alongside ibuprofen for better pain control.
Why is codeine dangerous while breastfeeding?
Codeine turns into morphine in your body, but some mothers-about 1 in 100-break it down too quickly. This can cause dangerously high morphine levels in breast milk, leading to severe breathing problems, extreme sleepiness, or even death in babies. The FDA warns against using codeine while breastfeeding because you can’t predict who will have this reaction.
Can I take tramadol while breastfeeding?
No. Tramadol is not safe while breastfeeding. Its active metabolite, M1, can build up in breast milk and cause life-threatening respiratory depression in infants. The FDA has issued multiple warnings against its use in nursing mothers due to documented cases of infant deaths.
What’s the safest opioid for breastfeeding mothers?
Morphine is the safest opioid for breastfeeding mothers. Babies absorb less than 1% of the morphine in breast milk, and it’s less likely to cause sedation. It’s preferred over oxycodone, hydrocodone, or any other opioid. Always use the lowest dose for the shortest time possible.
Do I need to pump and dump after anesthesia?
No. The idea that you need to pump and dump after anesthesia is outdated. Most anesthetics clear from your system quickly, and the tiny amounts in breast milk don’t harm your baby. You can breastfeed immediately after waking up. Early breastfeeding helps your recovery and reduces your need for pain meds.
How long should I use opioids after delivery?
Limit opioid use to 4-6 days maximum. Longer use increases the risk of dependency and infant sedation. If pain continues beyond a week, talk to your doctor about alternatives like physical therapy, heat, ice, or pelvic floor rehab. Don’t rely on opioids long-term.
Can I take naproxen while breastfeeding?
Naproxen is not recommended for breastfeeding mothers, especially in the first few weeks. It stays in your system longer and can build up in breast milk to levels that may affect your baby’s digestion or cause drowsiness. Stick to ibuprofen instead.

Declan Flynn Fitness
December 2, 2025 AT 08:39Just had my second kid last month and this post saved my sanity. Acetaminophen + ibuprofen combo? Absolute game changer. Took them alternating like clockwork-no sleep? No problem. Baby stayed alert, fed like a champ. No pump and dump needed. Seriously, why do doctors still push tramadol? 🤦♂️
ANN JACOBS
December 4, 2025 AT 05:23As a perinatal nurse with over 18 years of clinical experience, I cannot overstate the importance of evidence-based pharmacology in the postpartum period. The relative infant dose (RID) metrics cited herein are not merely anecdotal-they are derived from longitudinal, peer-reviewed pharmacokinetic studies conducted by the Academy of Breastfeeding Medicine and corroborated by the FDA’s 2018 pharmacovigilance reports. It is imperative that clinicians and patients alike prioritize pharmacodynamic safety over convenience, particularly when considering cytochrome P450 polymorphisms in opioid metabolism.
Kshitij Shah
December 4, 2025 AT 20:17Lmao. Americans think they invented pain management. In India, we’ve been using turmeric paste, cold compresses, and chai since forever. But hey, if you wanna pop pills like candy, go ahead. Just don’t tell me your baby’s sleepy because you took ‘morphine like a pro’.
Patrick Smyth
December 6, 2025 AT 13:11I just want to say-I’m a dad. My wife went through hell after the C-section. We were terrified of every pill. I read this whole thing out loud to her at 3 a.m. while she was crying from pain. She cried harder… but this time from relief. Thank you. From the bottom of my heart.
Nnaemeka Kingsley
December 6, 2025 AT 22:21bro this is gold. i had tramadol after my girl and she slept 20 hrs straight. i thought she was just tired. turns out she was almost dead. now i know. thanks man. share this everywhere.
Walker Alvey
December 7, 2025 AT 20:17Of course the medical establishment has a 12-page pamphlet on this. Meanwhile, my grandma healed with salt water and silence. You’re not healing-you’re medicating your way into dependency. Wake up.
Michelle Smyth
December 8, 2025 AT 04:13How delightfully reductive. The entire discourse around postpartum analgesia has been co-opted by a neoliberal pharmacopeia that pathologizes natural physiological processes. One must interrogate the epistemic violence inherent in privileging RID metrics over embodied maternal intuition. The very notion of ‘safe dosing’ assumes a Cartesian split between mother and child-an ontological fallacy, really. Isn’t it more radical to embrace the somatic wisdom of ancestral lactation practices? Or are we too enamored with our pillboxes to consider the silence between contractions?
Jaswinder Singh
December 9, 2025 AT 10:58Why the fuck are we still having this conversation? Codeine and tramadol are death traps. If your doctor prescribes them, fire them. Simple. No debate. No ‘maybe’. This isn’t a suggestion-it’s a survival guide. And yes, morphine is fine if you’re in real pain. Stop being scared. Your baby is tougher than you think.
Linda Migdal
December 10, 2025 AT 00:51Look, I get it. You want to ‘breastfeed your way to wellness.’ But in America, we don’t play games with our children’s lives. If you’re taking anything that’s not FDA-approved for lactation, you’re gambling. This isn’t Europe. We have standards. Stick to the list. No exceptions. Your baby’s brain is worth more than your pride.
Bee Floyd
December 10, 2025 AT 20:12Just wanted to say-this post felt like someone handed me a flashlight in a dark room. I was so overwhelmed after my C-section. I thought I had to choose between pain and bonding. Turns out, I could have both. Took morphine at 9 p.m., fed at 11. Baby slept like a angel. I cried. Not from pain-from gratitude. Thank you for writing this.
Matt Dean
December 11, 2025 AT 14:08Wow. Someone actually did the research. Who even are you? This isn’t some Instagram mom blog. This is legit. I’m saving this for my sister. She’s due next month. And yes, I’m sending it to her OB. She needs to stop listening to TikTok midwives.
James Steele
December 12, 2025 AT 21:23The pharmacokinetic profiles of NSAIDs in human milk are not merely ‘low’-they are statistically insignificant when contextualized within the ontogeny of neonatal hepatic metabolism. Moreover, the CYP2D6 ultra-rapid metabolizer phenotype exhibits a population prevalence of 1-2% in Caucasian cohorts, rendering population-wide contraindications both scientifically robust and ethically imperative. One must question the institutional inertia that still permits tramadol prescriptions in maternity wards.
Adrian Barnes
December 13, 2025 AT 20:00It’s not about safety. It’s about responsibility. If you can’t manage pain without risking your child’s life, then perhaps you shouldn’t be breastfeeding. There are formula options. There are adoption options. There are choices. You’re not a martyr. You’re a parent. Act like one.
Tommy Walton
December 14, 2025 AT 11:45Acetaminophen + ibuprofen = 🚀 Codeine = ☠️ Morphine = 🤝 Naproxen = 🚫 Pump and dump = 🤡 Save this. Share this. Live this.
Declan Flynn Fitness
December 15, 2025 AT 03:32^^^ This. And if you’re still reading this and thinking ‘I’ll just take one pill’-no. One pill is all it takes. I’ve seen it. My cousin’s baby went into respiratory arrest from tramadol. She didn’t even know she was a rapid metabolizer. Don’t be her.