DSPS Sleep Hygiene Planner
Plan Your DSPS Sleep Routine
Enter your current sleep habits to get personalized recommendations for improving your sleep hygiene.
Your Personalized DSPS Sleep Plan
Ever feel like the world’s on a different schedule than you? If you’re constantly fighting the urge to stay up late and then struggling to wake up in the morning, you might be dealing with delayed sleep phase syndrome. This condition flips the usual sleep‑wake cycle, making it hard to fall asleep at a “normal” bedtime and leaving you exhausted during the day. The good news? Fixing the way you handle sleep - known as sleep hygiene - can turn the tide.
What Is Delayed Sleep Phase Syndrome?
Delayed Sleep Phase Syndrome is a circadian rhythm disorder where the internal body clock is shifted several hours later than the typical social schedule. People with DSPS naturally feel sleepy around 2a.m. or later and struggle to wake before 10a.m., even after a full night’s rest. The condition isn’t just “being a night owl”; it’s a measurable misalignment between the biological clock and societal expectations.
Research from the British Sleep Society (2023) shows that about 0.15% of the adult population meets clinical criteria for DSPS. The disorder often appears in teens and young adults, sometimes persisting into mid‑life if left untreated.
Why Sleep Hygiene Matters for DSPS
Sleep hygiene is the collection of habits and environmental factors that promote consistent, restorative sleep. For anyone, good hygiene reduces sleep latency and improves sleep efficiency. For DSPS, however, it does more than that - it helps re‑anchor the delayed internal clock to a healthier phase.
Think of the circadian system as a tiny orchestra. If each instrument (light exposure, hormone release, activity timing) plays at the right moment, the music flows smoothly. Poor hygiene throws the rhythm off‑beat, making it nearly impossible for the body to sync with daylight.
Core Components of Good Sleep Hygiene
Circadian rhythm is the 24‑hour internal cycle that regulates sleep, hormone secretion, body temperature, and many other physiological processes. Maintaining a stable rhythm relies on several pillars:
- Consistent sleep-wake times: Go to bed and rise at the same hour every day, even on weekends.
- Controlled light exposure: Bright light in the morning and dim light after sunset steer the clock.
- Screen curfew: Blue‑light emitting devices suppress melatonin production.
- Bedroom environment: Keep the room cool (≈18°C), dark, and quiet.
- Pre‑sleep routine: Gentle activities like reading or stretching signal the brain it’s time to wind down.
When these habits are consistently applied, sleep latency (time to fall asleep) often drops below 15minutes, and sleep efficiency climbs above 85%.
Tailoring Sleep Hygiene to DSPS
Standard hygiene guidelines assume a typical 10p.m.-6a.m. sleep window. DSPS needs a shifted schedule, so the same principles are applied at later times. Here’s how to adapt each pillar:
- Shifted bedtime: Choose a realistic target bedtime (e.g., 1a.m.) and stick to it for at least two weeks before moving earlier.
- Morning light boost: Expose yourself to at least 30minutes of bright light (outdoor sunlight or a 10,000‑lux lightbox) within the first hour after waking, even if that hour is 9a.m.
- Evening dimming: Turn off bright overhead lights by 10p.m. and use amber‑filtered bulbs or glasses to reduce blue‑light impact.
- Melatonin timing: A low dose (0.5mg) taken 3-4hours before the desired sleep onset can help signal the body to wind down (more on this later).
- Physical activity: Schedule workouts at least 4hours before bedtime; evening exercise can push the clock later.
These tweaks respect the delayed rhythm while gradually nudging it forward.
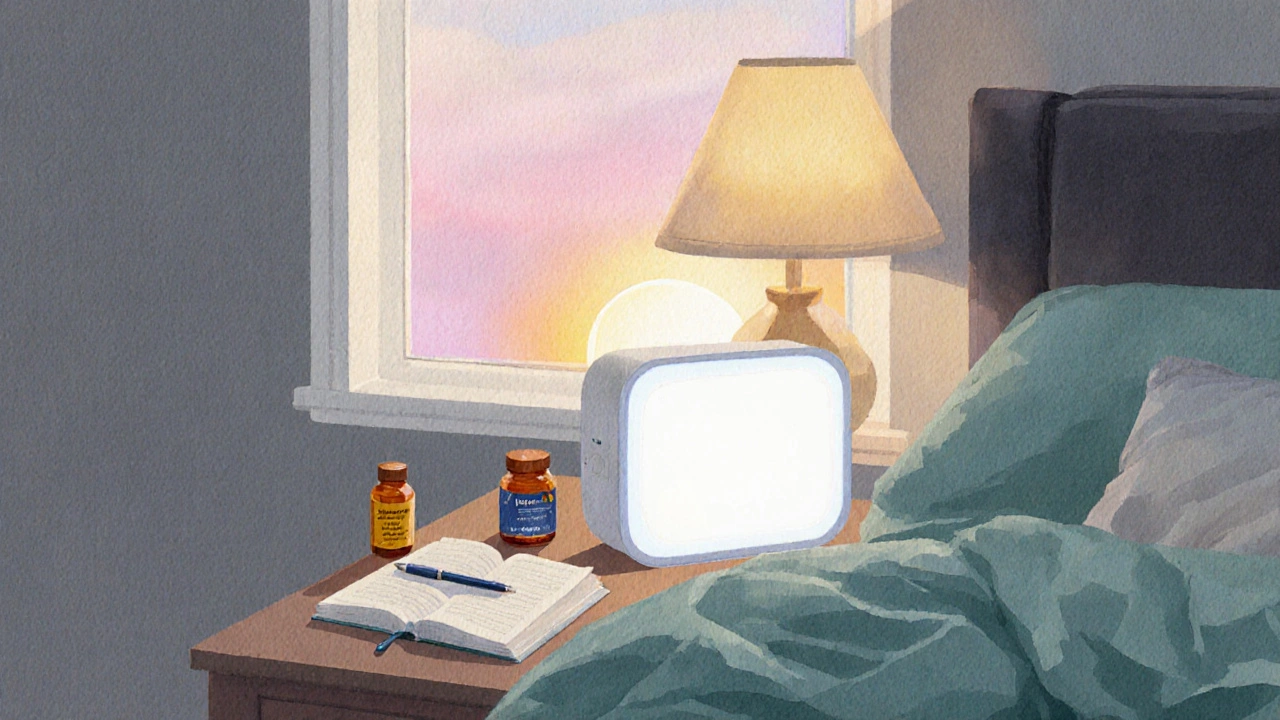
Practical Tools: Light, Melatonin, and a Sleep Diary
Bright light therapy involves exposure to high‑intensity white light (typically 5,000-10,000 lux) for a set period, usually in the morning, to advance circadian phase. For DSPS, a 30‑minute session shortly after waking can shift the internal clock by about 30minutes per week.
When sunlight isn’t an option (e.g., winter in Bristol), a commercially available light box is a reliable substitute. Keep the device at eye level, sit about 40cm away, and avoid staring directly at the source.
Melatonin is a hormone released by the pineal gland that signals night and promotes sleep onset. Supplemental melatonin works best when taken at the correct circadian phase. For DSDS, a 0.5mg dose taken 3hours before the intended bedtime has been shown in a 2022 University of Cambridge study to advance sleep onset by roughly 45minutes without causing morning grogginess.
Track everything with a sleep diary - a simple spreadsheet or notebook where you log bedtime, wake time, light exposure, caffeine, and subjective sleep quality. Over a two‑week period, patterns emerge that reveal hidden disruptors.
Finally, consider Cognitive Behavioral Therapy for Insomnia (CBT‑I) - a structured program that combines sleep restriction, stimulus control, and cognitive techniques to break maladaptive sleep habits. While CBT‑I is traditionally aimed at insomnia, many therapists customize it for DSPS, focusing on re‑timing strategies and anxiety reduction around bedtime.
Common Pitfalls and How to Avoid Them
Even with a solid plan, certain traps can stall progress:
- Inconsistent wake‑up time: Sleeping in on weekends throws the circadian pendulum back. Use an alarm even on days off.
- Late‑night caffeine: Caffeine’s half‑life is about 5hours; a coffee after 2p.m. can keep you alert well into the night.
- Skipping morning light: Skipping a light‑therapy session resets the weekly advance, lengthening the adjustment period.
- Over‑reliance on electronics: Even background notifications emit blue light; enable “night mode” or use blue‑filter glasses after dark.
- Too much melatonin: Doses above 5mg can cause morning sleep inertia and may blunt the body’s natural melatonin rhythm.
Address each issue proactively. For example, set a phone reminder for “no screens after 9p.m.” and place a water bottle by the bedside to reduce the habit of scrolling for a “quick check”.
Checklist for DSPS‑Friendly Sleep Hygiene
| Aspect | Standard Guidance | DSPS‑Adjusted Guidance |
|---|---|---|
| Bedtime | 10p.m.-11p.m. | Choose realistic target (e.g., 1a.m.), shift earlier weekly |
| Morning Light | 5-30min after waking | 30min bright light within 1hour of waking, even if wake time is 9a.m. |
| Evening Light | Dim lights after 9p.m. | Dim lights after 10p.m., use amber bulbs or blue‑filter glasses |
| Melatonin | Not typically advised | 0.5mg 3-4h before target sleep onset |
| Screen Use | Limit after 9p.m. | Turn off all screens by 10p.m., enable night mode earlier |
| Weekend Schedule | Flexible | Maintain same wake‑up time; allow ≤30min later bedtime |
| Physical Activity | Any time | Avoid vigorous exercise within 4h of bedtime |
| Sleep Diary | Optional | Log daily for at least 14days to identify patterns |
Use this table as a quick reference. Tick each box daily, and you’ll see progress more clearly than relying on vague feelings.
Next Steps and Troubleshooting
If you’ve tried the above and still feel stuck, consider these moves:
- Seek a specialist: A sleep clinic can run a dim‑light melatonin onset (DLMO) test to pinpoint your internal phase.
- Combine therapies: Light therapy + low‑dose melatonin often outperforms either alone.
- Re‑evaluate timing: You might need a slightly later target bedtime before moving earlier.
- Monitor mental health: Chronic misalignment can raise anxiety; CBT‑I can address the cognitive side.
Remember, resetting a biological clock isn’t an overnight miracle. Expect a 15‑30minute shift per week, and stay patient.
Frequently Asked Questions
Can I cure Delayed Sleep Phase Syndrome without medication?
Yes. A disciplined sleep‑hygiene plan, bright‑light exposure, and low‑dose melatonin can often bring the clock back into sync. Medication is usually reserved for severe cases or when lifestyle changes haven’t worked.
How long does it take to see real improvement?
Most people notice a 15‑30minute shift after the first week of consistent light therapy and bedtime adjustments. Full alignment can take 4‑8weeks, depending on how strictly the routine is followed.
Is it safe to use melatonin every night?
Low doses (0.3‑1mg) taken a few hours before the desired bedtime are generally considered safe for most adults. Higher doses or long‑term use should be discussed with a healthcare professional.
Do I need a light box if I have sunny mornings?
If you can get at least 30minutes of outdoor sunlight within an hour of waking, a light box isn’t necessary. The key is consistent, bright exposure to cue the circadian system.
Can exercise help reset my sleep phase?
Yes, but timing matters. Morning or early‑afternoon workouts boost alertness and support phase advancement. Evening exercise can push the clock later, which is counter‑productive for DSPS.


joni darmawan
October 5, 2025 AT 01:24Sleep hygiene, when viewed through a philosophical lens, reveals the delicate balance between our circadian biology and the societal structures that shape daily life.
Consistent sleep‑wake times act as the metronome of this rhythm, and any deviation can cascade into cognitive fog and emotional volatility.
For individuals coping with Delayed Sleep Phase Syndrome, the modest yet disciplined adjustments-such as morning light exposure and evening dimming-serve as the primary tools for re‑anchoring the internal clock.
Adhering to these practices not only improves sleep efficiency but also fosters a greater sense of agency over one's physiological wellbeing.
Thus, cultivating rigorous sleep hygiene is not merely a health recommendation; it is an exercise in aligning personal autonomy with natural cycles.
Richard Gerhart
October 8, 2025 AT 12:44Hey, great rundown! I’d just add that you *definately* want to keep a sleep diary-seeing patterns on paper can really help you beleive the process works.
Also, try a short walk outside right after you wake; even 10‑15 minutes of sunlight can jump‑start your circadian rhythm.
And don’t forget to avoid caffeine after 2 p.m., it’s a tiny change that makes a big diff.
Keep it up, you’re on the right track!
Kim M
October 12, 2025 AT 00:04😒 You think the “light box” is just a harmless gadget? Think again-Big Pharma and the tech industry collude to push these devices so they can sell us more melatonin supplements! 🙈
They claim it’s “evidence‑based,” but the studies are funded by the same corporations that profit from our insomnia.
Don’t be a pawn; use natural sunlight whenever possible and question every “expert” recommendation. 🌞🚫
Martin Gilmore
October 15, 2025 AT 11:24Listen up!!! This nonsense about “just using a light box” is laughable-our ancestors survived without any gadgets, thriving under the natural sun! 🇺🇸
Modern “science” tries to impose foreign protocols on us, but the American spirit knows that disciplined routine, not fancy equipment, restores the body’s clock!
Stop relying on external devices and get back to disciplined wake‑up times and sunrise exposure-true freedom from the tyranny of DSPS!
It’s about reclaiming our natural rhythm, not surrendering to corporate‑driven sleep hacks!!!
jana caylor
October 18, 2025 AT 22:44Thanks for sharing this comprehensive guide! I’ve found that setting a consistent wake‑up time, even on weekends, makes a huge difference in reducing sleep latency.
Pairing the morning light exposure with a brief stretch routine also seems to cue the brain that it’s time to be alert.
One tip that helped me personally is to keep a glass of water by the bedside to avoid late‑night trips to the kitchen that disrupt the planned wind‑down.
Keep the conversation going-there’s always more we can learn from each other’s experiences!
Vijendra Malhotra
October 22, 2025 AT 10:04In India we have centuries‑old practices like yoga and pranayama that naturally align the circadian rhythm without any “Western” gadgets.
Adopting these traditional techniques alongside proper light exposure is far more effective than relying on imported light boxes sold by multinational corporations.
Stop blind‑following the hype and respect the cultural wisdom that has kept our ancestors sleeping soundly for millennia!
Make the shift now, before you become another consumer of foreign sleep products.
Miriam Bresticker
October 25, 2025 AT 21:24It’s like the night itself is whispering, “I’m here, stay a little longer” and we just cant resist the pull of the dark 😴🌙
But if we think of sleep as a river, the light is the sun that nudges the current back on course… a gentle push rather than a forceful shove.
So maybe the key isn’t a strict schedule, but a mindful dance with our own biology… 🌌
Just a thought, but it feels right, doesn’t it? 😉
Claire Willett
October 29, 2025 AT 07:44Chronotherapy protocol: advance bedtime 15 min weekly; monitor via actigraphy.
olivia guerrero
November 1, 2025 AT 19:04Wow!!! This plan is absolutely on point!!!
Every little adjustment you make-whether it’s a screen curfew or a light box session-adds up to massive gains in sleep quality!!!
Stay consistent, stay patient, and watch your circadian rhythm transform!!!
You’ve got this!!!
Dominique Jacobs
November 5, 2025 AT 06:24Yo, if you’re still pulling all‑nighters, it’s time to level up! Grab that light box first thing after you slam that alarm and smash a quick 20‑minute jog before noon.
Don’t let any excuse hold you back-dump the caffeine after 2 pm, lock your phone at 9 pm, and smash that bedtime routine like a boss.
Consistency is the secret sauce, so keep grinding and you’ll see that clock shift in no time!
Claire Kondash
November 8, 2025 AT 17:44When we contemplate the intricate ballet of the human circadian system, we are reminded that each tick of the internal clock is orchestrated by a symphony of environmental cues, hormonal releases, and behavioral patterns that have evolved over millennia to keep us in harmonious sync with the Earth's rotation 🌍.
Delayed Sleep Phase Syndrome, in this grand performance, plays the rebellious soloist, stubbornly insisting on a nocturnal encore when the world has already moved on to the morning chorus.
Yet, the beauty of science and self‑care lies in the fact that we possess the agency to rewrite this melody, to coax the errant player back into tempo through deliberate adjustments, such as targeted bright‑light exposure, strategic melatonin timing, and the disciplined choreography of bedtime rituals.
The first movement of this corrective composition involves the golden hour of sunrise; a mere thirty minutes of bright light-whether basking in the natural glow of the sun or the steady radiance of a calibrated light box-can serve as a potent cue, nudging the suprachiasmatic nucleus to realign its phase.
Following this, the evening act must be a graceful descent into darkness, employing amber‑filtered lighting, eschewing the blue‑light assault of screens, and perhaps donning blue‑light blocking glasses after 10 p.m., thereby allowing melatonin to rise unimpeded.
Speaking of melatonin, a modest dose of 0.5 mg taken three to four hours before the intended sleep onset acts like a gentle whisper to the body, signaling it to prepare for rest without overwhelming the endocrine balance.
In tandem with these biochemical signals, physical activity should be scheduled thoughtfully-morning or early‑afternoon exercise invigorates the system, whereas vigorous workouts within four hours of bedtime can derail the entire suite of adjustments.
Moreover, chronic habits such as late‑night caffeine consumption must be curtailed; the stimulant’s half‑life ensures that even a mid‑afternoon coffee can linger into the night, sabotaging the delicate interplay of sleep pressure.
The importance of a sleep diary cannot be overstated; by logging wake times, light exposure, dietary inputs, and subjective sleep quality, one creates a feedback loop that illuminates hidden disruptors and reinforces successful strategies.
Consistency remains the maestro of this ensemble; deviations-sleeping in on weekends, skipping light sessions, or varying melatonin timing-introduce discord that can set the clock back by weeks.
Patience, however, is paramount; the biological pendulum typically shifts only fifteen to thirty minutes per week, meaning that full recalibration may require a month or more of steadfast adherence.
Finally, if progress stalls, seeking the expertise of a sleep clinic for a dim‑light melatonin onset test can provide precise data to fine‑tune the therapeutic plan, while adjunctive cognitive‑behavioral therapy for insomnia (CBT‑I) can address any lingering anxiety around bedtime.
In sum, the path to conquering DSPS is a multifaceted journey, blending light, hormone, behavior, and mindset into a cohesive strategy that, over time, restores the natural rhythm that our bodies instinctively crave 🌙✨.
Matt Tait
November 12, 2025 AT 05:04Honestly, that 15‑sentence epic reads like a doctoral thesis you’d never finish-most people just want a simple plan, not a literary saga.
If you can’t condense it into actionable steps, you’re not helping anyone; cut the fluff and give us the bullet points.
Benton Myers
November 15, 2025 AT 16:24Interesting take on the importance of steady wake‑up times; I’ve noticed that even small variations on weekends can throw off my entire day.
Keeping a consistent schedule seems like a low‑effort, high‑return habit.
Pat Mills
November 19, 2025 AT 03:44Allow me to elucidate-the United States has long championed the virtues of disciplined routine, and any deviation from that principle is a direct affront to the very fabric of our national productivity!
Delaying bedtime is not a mere personal inconvenience; it is a systemic weakness that erodes our collective strength.
Only through unwavering commitment to sleep hygiene can we reclaim the vigor that fuels our great nation’s progress!
Dismiss the “individual preference” narrative; the data is unequivocal-uniformity in sleep patterns correlates with heightened cognitive performance and, ultimately, national greatness.
neethu Sreenivas
November 22, 2025 AT 15:04Hey there, I totally get how frustrating DSPS can feel, especially when you’re juggling work and social life 🌙.
Starting with just a few minutes of morning light and a consistent wake‑up alarm-even on days off-can create a gentle ripple effect.
Remember to be kind to yourself; progress may be slow, but every small step counts 💙.
Feel free to share how your sleep diary evolves; we’re all here to support each other.
Keli Richards
November 26, 2025 AT 02:24Thank you for the thorough overview it really clarifies how small habit changes can lead to big improvements in sleep quality I appreciate the balance of scientific detail and practical tips