Parkinson's Medication Selector
Personalized Medication Recommendation
This tool helps determine the most appropriate Parkinson's medication based on your specific symptoms, age, and cognitive status. Select your characteristics to see which drug aligns best with your situation.
Your Personalized Recommendation
Common Side Effects
- Blurred vision
- Constipation
- Urinary retention
- Confusion
Did you know that over 10% of people with Parkinson's disease (PD) start on an anticholinergic drug like Trihexyphenidyl to control tremor? While it’s been around for decades, newer agents such as levodopa and dopamine agonists dominate today’s prescribing patterns. If you’re a patient, caregiver, or clinician trying to decide which pill fits best, you need a clear side‑by‑side look at how these drugs differ in effectiveness, safety, and practical use.
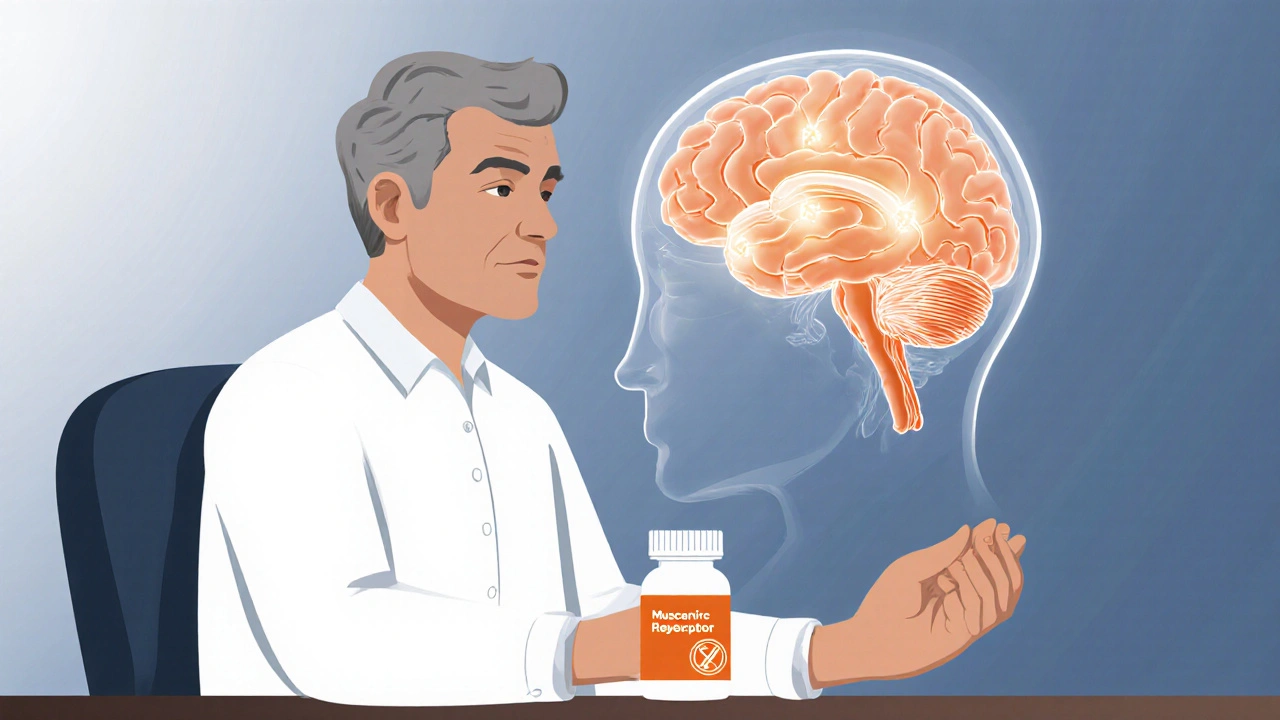
What Trihexyphenidyl Actually Does
Trihexyphenidyl is an anticholinergic medication that blocks muscarinic receptors in the brain, reducing excessive acetylcholine activity that contributes to tremor and rigidity. It was first approved in the 1950s and remains the go‑to oral anticholinergic for PD tremor, especially in younger patients who can tolerate its cognitive side effects.
Mechanistically, trihexyphenidyl restores the balance between dopamine and acetylcholine in the striatum. By dampening cholinergic overdrive, it smooths out the rhythmic shaking that often appears early in the disease. The drug is typically started at a low dose (1mg at bedtime) and titrated up to 10mg daily, split into two doses to minimize dry‑mouth and constipation.
How the Most Common Parkinson’s Drugs Work
Levodopa is the gold‑standard precursor to dopamine that, once converted in the brain, directly replenishes depleted dopamine levels. Usually combined with a peripheral decarboxylase inhibitor (carbidopa or benserazide) to prevent conversion outside the brain, levodopa offers the strongest symptomatic relief for bradykinesia and rigidity.
Ropinirole is a non‑ergoline dopamine agonist that stimulates D2/D3 receptors, mimicking dopamine’s effect without needing conversion. It’s often used early in the disease to delay levodopa initiation and smooth out motor fluctuations.
Benztropine is another anticholinergic, chemically similar to trihexyphenidyl, but with a slightly shorter half‑life and a higher propensity for causing dry eyes. It’s less commonly prescribed now because trihexyphenidyl offers once‑daily dosing for many patients.
Selegiline is a selective monoamine oxidase‑B (MAO‑B) inhibitor that blocks dopamine breakdown, modestly extending the effect of endogenous dopamine. It’s often added as an adjunct to levodopa to smooth out “off” periods.
Amantadine is an antiviral‑derived agent that releases dopamine and blocks NMDA glutamate receptors, useful for early‑stage motor symptoms and levodopa‑induced dyskinesia.
Key Differences at a Glance
| Medication | Drug Class | Primary Indication | Typical Starting Dose | Major Benefits | Common Side Effects | Best for |
|---|---|---|---|---|---|---|
| Trihexyphenidyl | Anticholinergic | Tremor‑dominant PD | 1mg nightly, titrate to 2-10mg/day | Reduces resting tremor, improves rigidity | Dry mouth, constipation, blurred vision, memory issues (especially >65y) | Younger patients with isolated tremor |
| Levodopa/Carbidopa | Dopamine precursor | General motor control | 100mg levodopa 3×/day | Strongest overall symptom relief | Nausea, orthostatic hypotension, motor fluctuations, dyskinesia | All stages, especially advanced PD |
| Ropinirole | Dopamine agonist | Early‑stage PD, “off” time reduction | 0.25mg BID, titrate to 4-8mg/day | Delays levodopa need, smoother motor response | Somnolence, nausea, impulse control disorders | Younger patients seeking levodopa sparing |
| Benztropine | Anticholinergic | Tremor & rigidity | 0.5mg BID | Similar tremor control as trihexyphenidyl | Dry mouth, urinary retention, confusion | Patients intolerant to trihexyphenidyl dosing schedule |
| Selegiline | MAO‑B inhibitor | Adjunct therapy | 5mg daily (tablet) or 10mg daily (patch) | Prolongs dopamine effect, reduces “off” periods | Hypertension crisis with tyramine foods (tablet), insomnia (patch) | Patients needing extra dopamine support without levodopa escalation |
| Amantadine | Antiviral‑derived dopaminergic | Early motor symptoms, dyskinesia | 100mg daily, titrate up to 300mg/day | Improves gait, reduces levodopa‑induced dyskinesia | Foot swelling, livedo reticularis, insomnia | Patients with troublesome dyskinesia |
When to Choose Trihexyphenidyl Over the Rest
Trihexyphenidyl shines in three scenarios:
- Isolated tremor: If rigidity and bradykinesia are mild, the drug can quiet the shaking without the motor fluctuations that come with levodopa.
- Younger age: Patients under 70 usually tolerate the cognitive side effects better, and the risk of long‑term anticholinergic dementia is lower.
- Contraindications to dopamine agents: Some individuals have severe nausea, cardiac issues, or prior dyskinesia that make dopamine‑based drugs a poor fit.
However, the decision isn’t just about age. A short cognitive screen (e.g., MoCA) can flag patients who might develop memory problems. If the score dips below 26, clinicians often pivot to a dopamine agonist or levodopa.
Managing Trihexyphenidyl’s Side Effects
Because the drug blocks acetylcholine, dry mouth is almost guaranteed. Simple tricks-sipping water, sugar‑free gum, or saliva‑stimulating lozenges-can keep comfort high. Constipation can be tackled with dietary fiber, plenty of fluids, and occasional stool softeners.
Blurred vision occurs from reduced pupillary constriction. A quick eye‑exam and lubricating drops usually solve the issue. The trickiest side effect is cognitive fog, especially at doses above 6mg/day. If a patient reports memory lapses, taper the dose by 1mg every few days while monitoring tremor control.
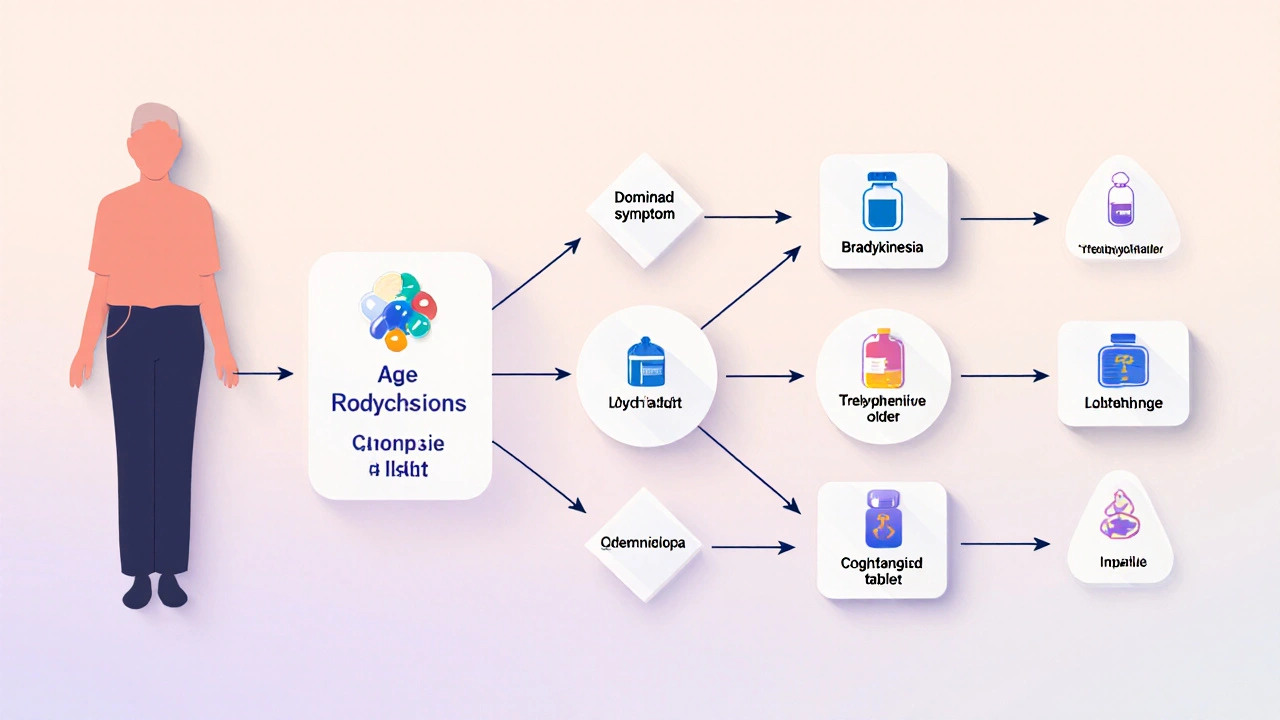
Putting It All Together: A Practical Decision Tree
- Identify the dominant symptom: tremor vs. bradykinesia vs. rigidity.
- Assess age and cognitive baseline.
- If tremor is primary and patient is <70y with good cognition → consider trihexyphenidyl.
- If motor slowing is prominent or patient is >70y → start levodopa or a dopamine agonist.
- For patients with early dyskinesia on levodopa → add amantadine.
- If adjunct dopamine‑preserving therapy is needed → add selegiline or rasagiline.
- Re‑evaluate every 3-6months; adjust doses or switch class based on side‑effect profile.
This flow keeps you from jumping straight to the most potent drug (levodopa) when a milder anticholinergic could suffice.
Frequently Asked Questions
Can trihexyphenidyl be used with levodopa?
Yes. Combining an anticholinergic with levodopa can improve tremor without drastically increasing levodopa‑related dyskinesia. Start levodopa at a low dose, add trihexyphenidyl only if tremor persists, and watch for additive dry‑mouth or constipation.
Why does trihexyphenidyl cause memory problems?
The drug blocks muscarinic receptors throughout the brain, including areas that handle learning and recall. Reduced acetylcholine transmission can temporarily slow information processing, especially in older adults.
Is trihexyphenidyl still prescribed in 2025?
Absolutely. While newer agents dominate, guidelines still list anticholinergics as first‑line for tremor‑dominant PD in patients under 70 without significant cognitive impairment.
What should I do if I experience severe dry mouth?
Increase water intake, use sugar‑free lozenges, and talk to your neurologist about a dose reduction or a switch to benztropine, which may have a slightly milder xerostomia profile.
Can I take trihexyphenidyl if I have glaucoma?
No. Anticholinergics can raise intra‑ocular pressure, worsening glaucoma. Patients with narrow‑angle glaucoma should avoid trihexyphenidyl and discuss alternative tremor treatments.
Bottom line: trihexyphenidyl remains a valuable tool for a specific slice of the Parkinson’s population-young, tremor‑dominant patients without cognitive risk. By weighing its benefits against the side‑effect spectrum and comparing it side‑by‑side with levodopa, dopamine agonists, and other adjuncts, you can craft a medication plan that balances symptom control with quality of life.

Jason Montgomery
October 16, 2025 AT 15:11Hey folks, just wanted to say that if you’re thinking about trying trihexyphenidyl, start low and go slow – 1 mg at night is a good launch point. Keep an eye on that dry mouth, a water bottle and sugar‑free gum are lifesavers. If constipation shows up, add a fiber supplement and stay hydrated. For younger patients the cognitive side‑effects are usually manageable, especially under 70. And don’t forget to reassess every few months – a dose tweak can keep the tremor in check without over‑doing the anticholinergic load.
Wade Developer
October 23, 2025 AT 00:51From a mechanistic perspective, trihexyphenidyl’s anticholinergic action restores the dopaminergic‑acetylcholinergic equilibrium in the striatum, thereby attenuating tremor. Comparative efficacy data suggest that while levodopa remains superior for bradykinesia, anticholinergics retain a niche for tremor‑dominant phenotypes. It is crucial to evaluate the patient's cognitive baseline using tools such as the MoCA before initiating therapy. The pharmacokinetic profile, with a half‑life of approximately 6–10 hours, supports bidirectional dosing in many cases. Nevertheless, clinicians must remain vigilant for peripheral anticholinergic adverse events, particularly in the elderly.
Sandra Perkins
October 29, 2025 AT 12:18Wow, another anticholinergic – just what the world needed, right?
rama andika
November 5, 2025 AT 00:45Oh sure, because the pharma overlords are totally not pulling strings to keep us on the newest dopamine‑boosters while they hide the ancient anticholinergics in the basement. It’s all a grand illusion, folks – the real tremor cure is a secret herbal brew that the “big pharma” can’t patent. But hey, if you trust the system, go ahead and pop the old‑school pill, just don’t expect miracles.
Kenny ANTOINE-EDOUARD
November 11, 2025 AT 13:12Let me walk through a practical roadmap for integrating trihexyphenidyl into a Parkinson’s regimen. First, assess the dominant motor symptom – if tremor outweighs bradykinesia, the anticholinergic axis becomes a front‑line option. Second, conduct a baseline cognitive screen; a MoCA score above 26 suggests the patient can tolerate the central anticholinergic load. Third, initiate at 1 mg nightly, monitoring for xerostomia and constipation, which are the most predictable peripheral side effects.
Fourth, if tremor persists after a week, consider a modest titration to 2 mg split as 1 mg morning and 1 mg evening, always keeping the total daily dose ≤10 mg to mitigate cognitive risk.
Fifth, educate the patient about simple mitigations: sugar‑free lozenges for dry mouth, a high‑fiber diet with adequate fluids for bowel health, and lubricating eye drops if blurred vision emerges.
Sixth, schedule a follow‑up at 4‑6 weeks to re‑evaluate tremor severity using the UPDRS tremor item and reassess cognition; a slight dip in MoCA (< 1‑point change) warrants a dose reduction.
Seventh, be prepared to combine with levodopa if tremor control remains suboptimal – the synergy can be beneficial, but watch for additive anticholinergic burden.
Eighth, consider switching to benztropine only if dosing convenience is a priority, as the side‑effect profile is largely overlapping.
Ninth, for patients over 70 or with pre‑existing memory issues, prioritize dopamine agonists or levodopa to avoid exacerbating cognitive decline.
Tenth, always counsel about the risk of intra‑ocular pressure elevation; a brief ophthalmology check is prudent in patients with glaucoma history.
Eleventh, document adverse events meticulously, as real‑world data on anticholinergic‑related falls remain limited.
Twelfth, involve caregivers in monitoring daily function – subtle executive dysfunction can be missed by the patient.
Thirteenth, if dyskinesia emerges while on levodopa, amantadine may be added; this does not interfere with trihexyphenidyl’s tremor‑control efficacy.
Fourteenth, keep an eye on drug‑drug interactions – anticholinergics can potentiate anticholinergic load from antihistamines and tricyclic antidepressants.
Fifteenth, remember that the therapeutic window narrows with disease progression; periodic reassessment is key.
Sixteenth, by following this structured approach, clinicians can harness the benefits of trihexyphenidyl while minimizing its pitfalls, ultimately preserving quality of life for tremor‑dominant patients.
Craig Jordan
November 18, 2025 AT 01:39Alright, let’s dissect this so‑called “roadmap” with a skeptic’s eye. First off, the emphasis on tremor‑dominant phenotypes ignores the reality that most Parkinson’s patients present with mixed motor features, making any single‑agent strategy simplistic at best. Second, the recommendation to titrate up to 2 mg split dosing feels overly cautious; many clinicians safely employ 4–6 mg once daily, especially in patients with robust hepatic clearance. Third, the advice to combine with levodopa to achieve synergy is a double‑edged sword – you may be trading one set of side effects for another, notably levodopa‑induced dyskinesia, a problem the original author downplays. Fourth, the claim that anticholinergics are safe under 70 lacks robust longitudinal data; studies have shown subtle memory deficits even in younger cohorts when followed beyond two years. Fifth, the suggestion to involve caregivers assumes that patients have that support system, which isn’t universally true. Sixth, the “ocular pressure” warning is valid but over‑emphasized; most patients tolerate the drug without routine ophthalmology checks. Seventh, the mention of “high‑fiber diet” is generic, failing to address the need for individualized bowel regimens in the context of polypharmacy. Eighth, the statement about benztropine’s dosing convenience is questionable, as its twice‑daily schedule is often comparable to trihexyphenidyl’s split dosing in practice. Ninth, the author’s dismissal of anticholinergic load from other meds seems naive – a comprehensive medication review is mandatory. Tenth, while the roadmap is thorough, it reads like a checklist rather than a nuanced clinical decision‑making process. In short, the guide is useful but needs more balance, more evidence, and less dogmatic phrasing.
carl wadsworth
November 24, 2025 AT 14:07Listen up – if you’re going to start trihexyphenidyl, you’ve got to be ruthless about dosing. No half‑measures. Begin at 1 mg at night, then crank it up to 5 mg split only if the tremor is still raging. Anything less and you’re just playing medical roulette. And quit whining about dry mouth; chew gum, sip water, period. If you can’t handle the side effects, you’re not cut out for this line of therapy. Get aggressive with the titration schedule and you’ll see results in a week.
Neeraj Agarwal
December 1, 2025 AT 02:34actually, the proper term is xerostomia, not dry mouth. also, proper grammar would be "if you can't handle" not "if you cant handle". just a heads up.
Rose K. Young
December 7, 2025 AT 15:01Seriously? Another post glorifying an old‑school drug while ignoring the massive cognitive toll it takes on patients? Wake up. The only thing worse than placebo is this antiquated anticholinergic nonsense. Anyone still prescribing this should be ashamed.
Christy Pogue
December 14, 2025 AT 03:28Hey everyone! 🌟 This guide is super helpful – love the clear tables and the decision tree. It makes figuring out the right med feel less intimidating. Keep the positivity coming!
Helena Pearson
December 20, 2025 AT 15:55👍 Absolutely! The depth here is impressive 😊. If we think about the neurochemical balance, trihexyphenidyl offers a nuanced approach that many overlook. But remember, the art of medicine isn’t just about charts – it’s about listening to the patient’s lived experience. 👂💊
Patricia Fallbeck
December 27, 2025 AT 04:22🚀 Wow, another “comprehensive guide”. 🙄 As if we needed another checklist. The real world is messy, not a tidy table. But hey, if you like crossing T’s and dotting I’s, go ahead and read it. 🎭
Brett Snyder
January 2, 2026 AT 16:49Patriots of neurology, hear me! Our brave doctors should champion the classic meds that made our forefathers strong. This fancy levodopa craze is just another foreign influence trying to undermine our medical heritage. Stand firm with trihexyphenidyl – it’s the real American solution.
Nidhi Jaiswal
January 9, 2026 AT 05:16i think the post is ok but maybe the author could add more on side effects typos are there but overall good
Sunil Sharma
January 15, 2026 AT 17:43Team, let’s remember that each patient is unique, so we should tailor the dosing schedule to the individual’s daily routine. Encouraging open dialogue with patients helps us adjust therapy quickly and safely.
Leah Robinson
January 22, 2026 AT 06:10Love seeing such a thorough breakdown! 🎉 It really helps demystify the choices we have. Thanks for putting this together – you’ve made my day! 😊
Abhimanyu Lala
January 28, 2026 AT 18:37Okay this is drama central – but hey, drug guide, got it.
Richard Sucgang
February 4, 2026 AT 07:04One must critique the syntactic laxity present throughout this exposition. The author neglects proper subjunctive constructions and, frankly, the prose verges on the pedestrian. Such editorial sloppiness undermines the scholarly gravitas the subject demands.