Progressive MS: What You Need to Know
If you or someone you love has been told they have progressive multiple sclerosis (MS), the first thought is often "what now?" Unlike relapsing‑remitting MS, progressive forms keep getting worse over time, with fewer clear flare‑ups. That can feel scary, but knowing the basics helps you stay a step ahead.
There are two main types: primary progressive (PPMS) shows steady decline from the start, while secondary progressive (SPMS) follows an earlier relapsing phase and then begins to worsen steadily. Both involve growing disability, but the speed varies person to person. The good news is that research is catching up fast, and there are more tools than ever to slow the march.
Common Signs and How They Change
The first clue of progressive MS is usually a gradual loss of function that doesn’t fully bounce back after a relapse. You might notice:
- Weakness or clumsiness in the legs that slowly gets worse.
- Balance problems – stumbling on flat ground, not just during an attack.
- Spasticity – muscles feel tight or jerky even when you’re resting.
- Pain and fatigue that don’t improve with rest.
- Cognitive fog – trouble remembering names, staying focused, or finding words.
These symptoms can appear one at a time or together. Because they develop slowly, families sometimes think it’s just aging. A neurologist can confirm progressive MS with MRI scans that show new lesions and brain‑spine shrinkage over months.
Managing Progression and Everyday Life
The goal isn’t cure (yet) but slowing the slope. Disease‑modifying therapies (DMTs) like ocrelizumab are approved for primary progressive MS, while siponimod works for secondary forms. Talk to your doctor about eligibility – many insurers now cover these drugs if you meet certain criteria.
Beyond meds, lifestyle makes a real difference:
- Exercise – low‑impact activities like swimming, cycling or yoga keep muscles strong and improve balance. Even short 10‑minute sessions help.
- Physical therapy – a therapist can teach you safe stretches and gait tricks to reduce falls.
- Nutrition – anti‑inflammatory foods (fatty fish, berries, leafy greens) support brain health. Stay hydrated; dehydration worsens fatigue.
- Sleep hygiene – aim for 7‑8 hours, keep the room cool, limit screens before bed.
- Stress control – meditation, deep breathing or a hobby can lower cortisol, which may slow disease activity.
Don’t forget mental health. Living with progressive MS can feel isolating, so join online communities or local support groups. Sharing tips on wheelchair ramps, adaptive tools and insurance tricks lifts everyone’s spirit.
If you’re starting a new treatment, keep a symptom diary. Note any changes in strength, walking distance, pain levels, or mood. This record helps your neurologist tweak the plan before problems get big.
Finally, stay curious about research. Clinical trials are testing remyelination drugs, stem‑cell approaches and advanced imaging to catch disease early. Ask your doctor if a trial fits your situation – many studies cover travel costs and medication.
Progressive MS is tough, but you’re not powerless. With the right meds, daily habits, and a solid support crew, you can keep moving forward and enjoy life’s moments on your terms.
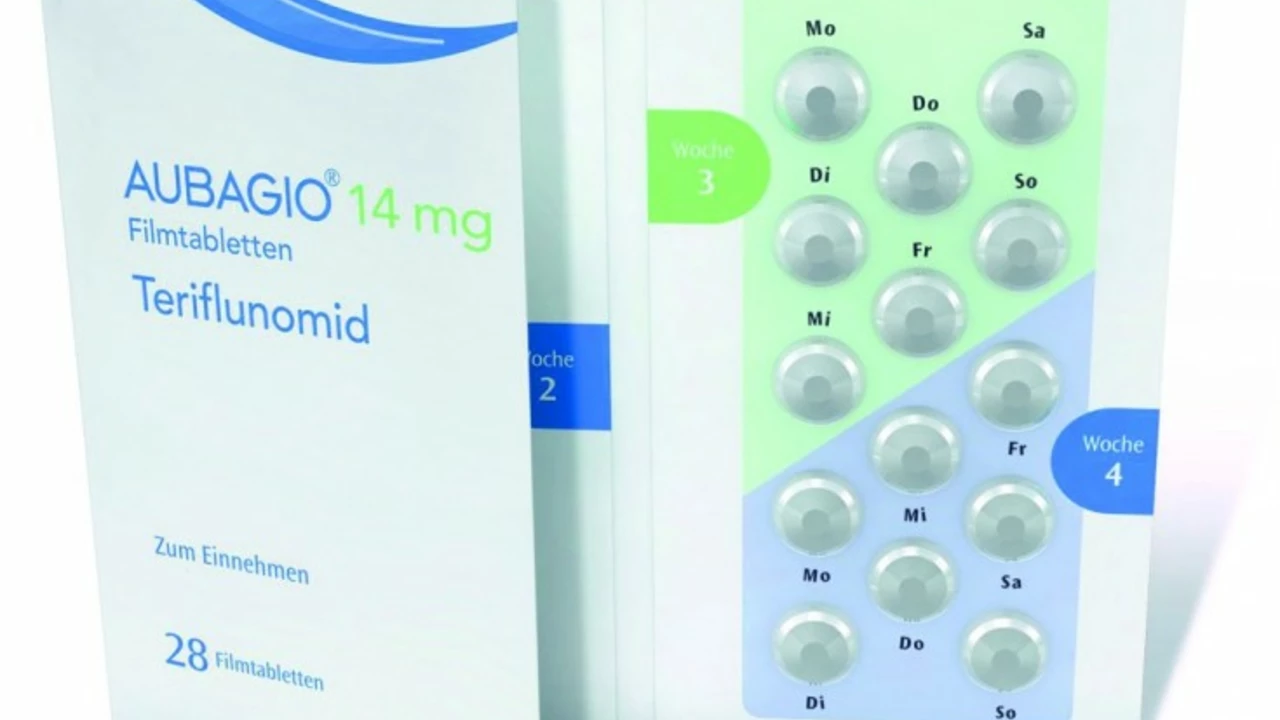
Teriflunomide and Progressive MS: Is There a Role for This Medication?
Jun, 28 2023
