MS Treatment Guide: What Works, What Doesn’t, and How to Start
If you or someone you know has been diagnosed with multiple sclerosis (MS), the first thing that comes to mind is probably “what now?” The good news is there are more treatment choices than ever before. From pills that slow disease progression to therapies that tackle fatigue, pain, and bladder issues, you can build a plan that fits your life.
First‑line disease‑modifying drugs
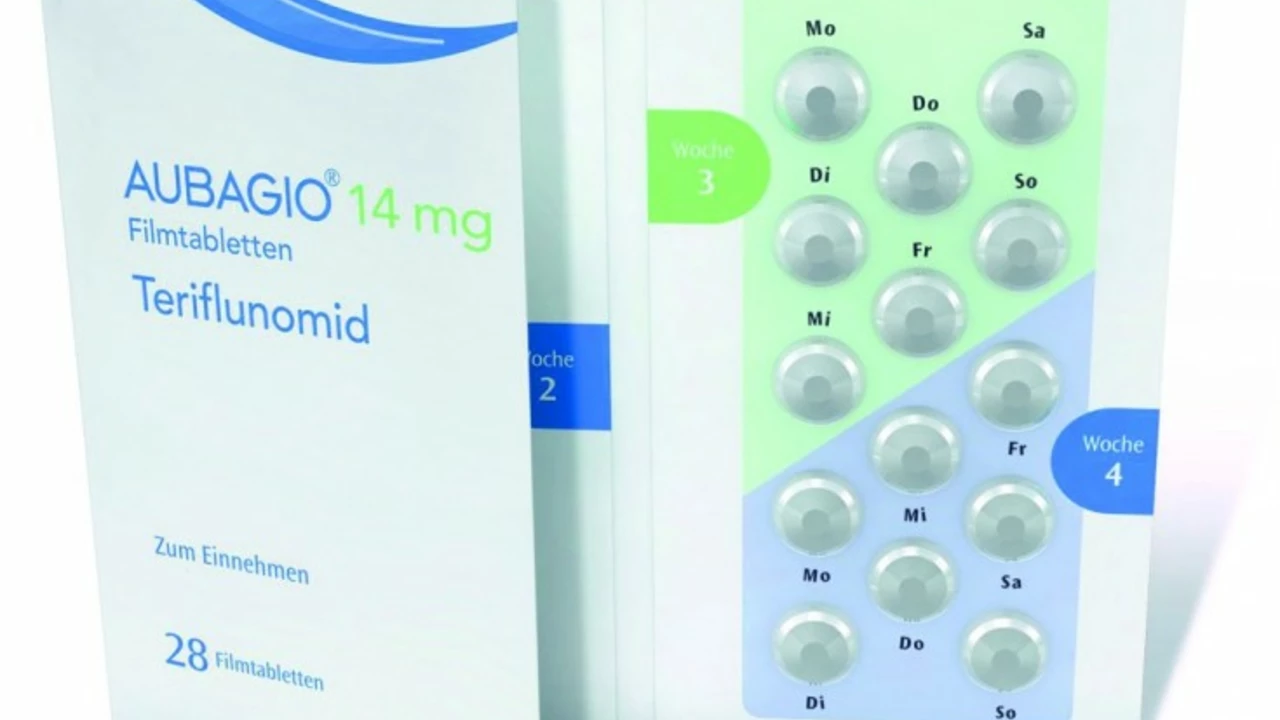
The backbone of modern MS care is disease‑modifying therapy (DMT). These medicines aim to reduce new lesions and keep relapses at bay. The most common oral options include fingolimod, dimethyl fumarate, and teriflunomide. If you prefer an injection, interferon beta‑1a or glatiramer acetate are still solid choices. For aggressive cases, doctors may suggest high‑efficacy infusions like natalizumab or ocrelizumab.
Choosing a DMT involves weighing factors such as side‑effects, how often you need to take the drug, and your personal health history. Talk with your neurologist about blood work requirements, liver monitoring, and any infection risks before committing.
Managing symptoms on top of DMTs
Even with a strong DMT, MS can bring fatigue, spasticity, pain, or bladder problems. Simple lifestyle tweaks—regular low‑impact exercise, a balanced diet rich in omega‑3s, and good sleep hygiene—can make a big difference.
For spasticity, physical therapy plus medications like baclofen or tizanidine often help. Pain that feels nerve‑related may respond to gabapentin or duloxetine. If bladder urgency is an issue, pelvic floor exercises and prescription anticholinergics can improve control.
Don’t overlook mental health. Depression and anxiety are common in MS, so counseling, support groups, or antidepressants deserve the same attention as any physical symptom.
When to consider a treatment change
If you notice more frequent relapses, MRI scans showing new lesions, or intolerable side‑effects, it’s time for a reassessment. Switching from a moderate‑efficacy DMT to a high‑efficacy option can halt disease activity faster. Your doctor may also suggest a “washout” period between drugs to avoid overlapping immune suppression.
Pregnancy adds another layer of decision‑making. Some DMTs are safe during pregnancy, while others require stopping months before conception. Always discuss family planning early on so you can map out a safe treatment schedule.
Practical steps to start your plan
1️⃣ Schedule a detailed appointment with an MS‑specialized neurologist. 2️⃣ Bring a list of current meds, allergies, and any recent lab results. 3️⃣ Ask about the pros and cons of each DMT option—focus on dosing schedule and monitoring needs. 4️⃣ Set up a baseline MRI and blood work so future changes can be measured accurately. 5️⃣ Create a symptom journal. Note fatigue levels, mobility issues, and mood shifts; this data guides adjustments.
Remember, MS treatment isn’t one‑size‑fits‑all. It’s a mix of disease control, symptom relief, and lifestyle support that evolves with you. Keep the conversation open with your care team, stay informed about new therapies, and don’t hesitate to tweak the plan as you learn what works best for your body.
Ready to take the next step? Start by booking a consult, gathering your health records, and jotting down any questions you have. The sooner you act, the more options you’ll have to keep MS in check and live life on your terms.
Teriflunomide and Progressive MS: Is There a Role for This Medication?
Jun, 28 2023
