FDA MedWatch: Understanding Drug Safety Reporting and What It Means for You
When you take a new medicine, you trust it’s been tested for safety. But the truth is, some side effects only show up after thousands of people start using it. That’s where FDA MedWatch, the U.S. Food and Drug Administration’s official system for collecting reports of harmful side effects from medications, medical devices, and other health products. Also known as MedWatch Safety Alerts, it’s the backbone of post-market drug safety in the United States. This isn’t just paperwork—it’s a real-time warning system that helps pull dangerous drugs off shelves or update labels with new risks.
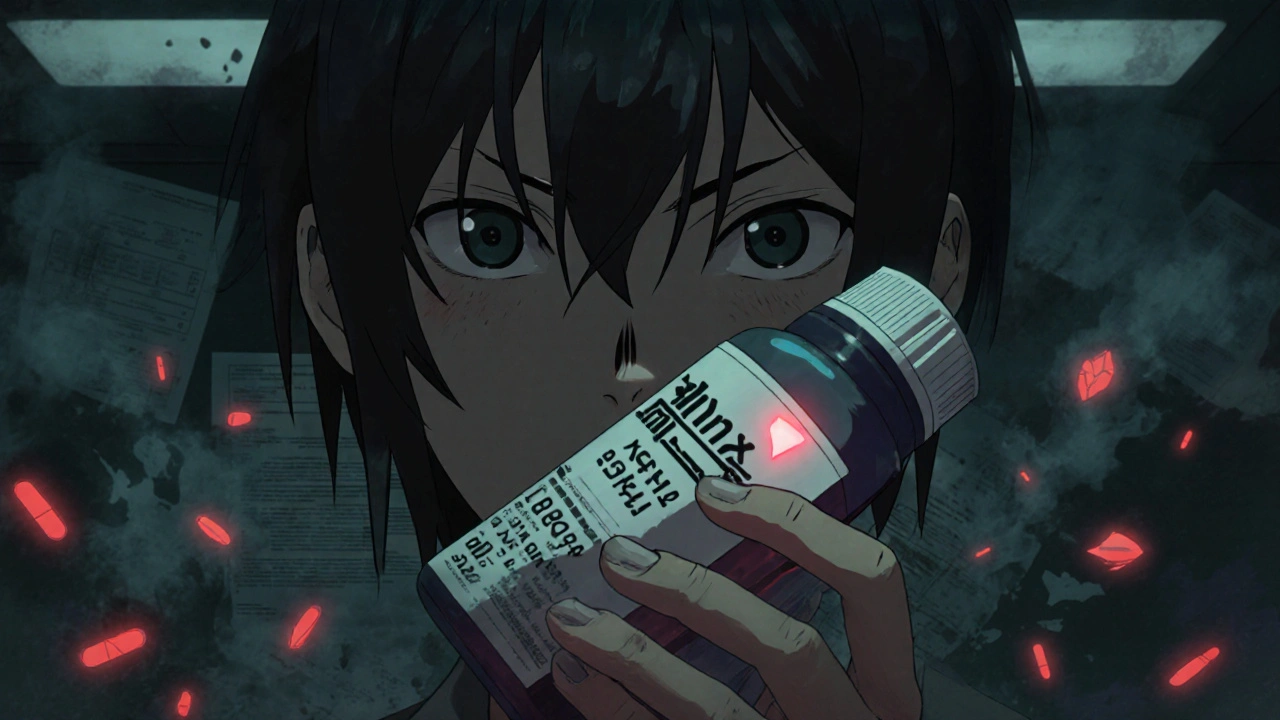
FDA MedWatch relies on two groups: healthcare providers and patients. Doctors, nurses, and pharmacists report serious reactions like liver failure, heart rhythms gone wrong, or sudden allergic responses. But patients matter too. If you or someone you know had a bad reaction to a pill, patch, or injection, your report can trigger an investigation. The FDA doesn’t just wait for labs to find problems—they listen to real people. That’s why reports of rare but deadly side effects, like the ones tied to certain painkillers or antidepressants, often start with a single patient’s call to their doctor or a form submitted online.
Related to this are adverse drug reactions, unintended and harmful effects caused by a medication at normal doses, which form the core of MedWatch data. These aren’t just nausea or dizziness—they’re events that land people in the hospital or cause permanent damage. Then there’s post-market surveillance, the ongoing monitoring of drugs after they’ve been approved and sold to the public. Unlike clinical trials, which involve a few thousand people over months, post-market surveillance watches millions over years. That’s how we found out about the heart risks with some weight-loss pills, or the suicide risk linked to certain antidepressants in young adults.
You might wonder why some drugs stay on the market even after reports come in. That’s because MedWatch doesn’t mean a drug is banned—it means the FDA is looking closer. Sometimes, they add stronger warnings. Other times, they restrict who can get it. And sometimes, they pull it entirely. The key is that these decisions aren’t made in secret. The public gets updates through MedWatch alerts, which you can sign up for free. You’ll know before your next refill if something changed.
What you’ll find in these posts isn’t just technical jargon—it’s real stories behind the numbers. You’ll learn how a single report led to changes in how insulin is labeled, how a patient’s note helped flag a dangerous interaction between two common heart drugs, and why generic versions of certain medications need extra scrutiny. You’ll also see how storage mistakes, mislabeled doses, and even handwriting errors tie into the bigger picture of drug safety. These aren’t abstract policies—they’re life-or-death details that affect what’s in your medicine cabinet right now.
FDA MedWatch isn’t something that happens in a lab far away. It’s happening every time someone speaks up. And if you’ve ever wondered why your doctor asks, ‘Have you noticed any new side effects?’—now you know. Your answer might help someone else avoid a serious reaction. The system only works if people use it. And the more you understand it, the better you can protect yourself and others.
How to Report Suspected Counterfeit Drugs to Authorities
Nov, 21 2025
