FDA-approved devices: What they are, how they work, and what to know before using them
When you see FDA-approved devices, medical tools and equipment cleared by the U.S. Food and Drug Administration for safe use in diagnosing, treating, or monitoring health conditions. Also known as regulated medical devices, they’re not just gadgets—they’re tools that have gone through strict testing to prove they work as claimed and won’t harm you when used properly. This doesn’t mean they’re perfect, but it does mean they’ve passed a system designed to keep people safe.
FDA-approved devices cover a huge range—from simple things like blood pressure monitors, home devices used to track hypertension and guide treatment decisions, to complex ones like insulin pumps, electronic systems that deliver precise doses of insulin for people with diabetes. You’ll also find nerve stimulators, implantable or wearable units that reduce chronic pain by interrupting pain signals, and even at-home diagnostic kits, tools that let you test for conditions like pregnancy, strep throat, or blood sugar levels without leaving your house. These aren’t just convenience items—they’re part of daily care for millions.
What makes a device FDA-approved isn’t just the brand or the price tag. It’s about the data: clinical studies, safety reports, and real-world performance. The FDA doesn’t approve every device the same way—some go through a fast-track review if they’re similar to existing ones, while others need full clinical trials. That’s why two devices that do the same thing might have very different levels of evidence behind them. Knowing this helps you ask better questions: Is this device backed by real testing? Has it been used by enough people to show it’s reliable? And is there a cheaper or simpler option that works just as well?
You’ll find posts here that compare specific devices to their alternatives—like how one pain relief patch stacks up against another, or why a certain glucose monitor is preferred over similar models. These aren’t marketing pieces. They’re real breakdowns of what works, what doesn’t, and what’s worth the cost. Whether you’re managing a long-term condition, looking for better symptom control, or just trying to avoid unnecessary spending, the information below gives you the facts without the fluff.
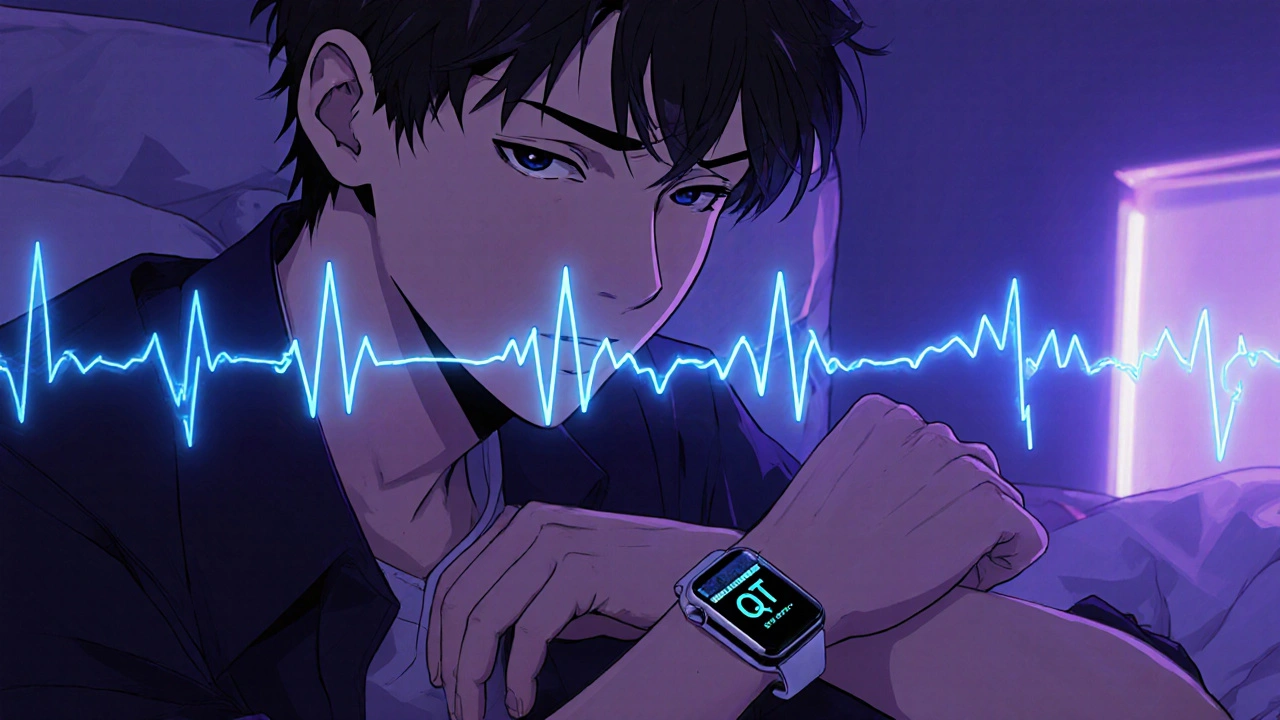
Real-Time QT Safety with Wearable ECGs: Detect Cardiac Risk Instantly
Oct, 25 2025
