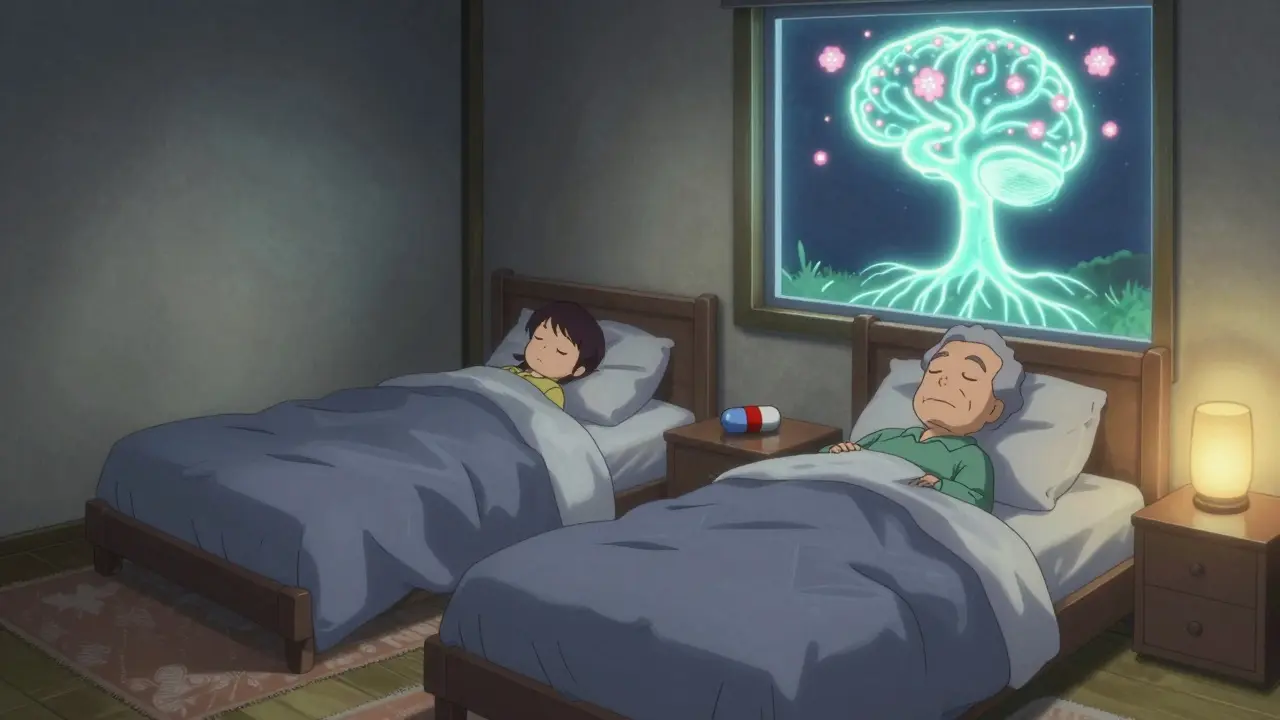
REM sleep behavior disorder isn’t just about dreaming loudly or kicking in your sleep. It’s a warning sign your brain is changing-possibly in ways that could lead to Parkinson’s disease, dementia with Lewy bodies, or other serious neurological conditions. People with RBD don’t just move during dreams; they punch, yell, jump out of bed, or even run into walls. And if left unaddressed, it can lead to serious injury-not just for the person with RBD, but for their partner too.
What Exactly Is REM Sleep Behavior Disorder?
During normal REM sleep, your body is paralyzed-except for your eyes and breathing muscles. This is called muscle atonia. It keeps you from acting out your dreams. In RBD, that paralysis fails. You’re awake in your mind, but your body isn’t getting the signal to stay still. So you act out vivid, often violent dreams: fighting off attackers, yelling at imaginary intruders, or flailing as if you’re running.
This isn’t occasional restlessness. It happens regularly-on average, 4.2 times per hour during REM sleep, according to sleep lab studies. And it’s not rare. About 1 in 500 adults have it. But most don’t know they have it until their partner wakes up bruised or calls 911 after a fall.
What makes RBD especially concerning is what it might predict. Around 90% of people with RBD will eventually develop a neurodegenerative disease. Studies show 73.5% of those with idiopathic RBD (meaning no known cause) will develop Parkinson’s, dementia with Lewy bodies, or multiple system atrophy within 12 years. That’s why doctors don’t just treat the symptoms-they watch for early signs of brain decline.
How Is RBD Diagnosed?
You can’t diagnose RBD with a blood test or an MRI. The only way to confirm it is through a sleep study called polysomnography (PSG). During this overnight test, electrodes track your brain waves, eye movements, muscle activity, heart rate, and breathing.
The key finding? REM sleep without atonia (RSWA). That means your muscles are active during REM sleep when they should be completely still. The International Classification of Sleep Disorders says RSWA must be present in at least 15% of REM sleep epochs to meet diagnostic criteria.
Doctors also look for other clues: dream enactment behaviors reported by a bed partner, no signs of seizures or other sleep disorders, and symptoms that aren’t caused by medications or substance use. If you’ve been told you “sleep like a fighter” or your partner says you’ve “become a different person at night,” it’s time to see a sleep specialist.
First-Line Medications: Melatonin and Clonazepam
There are no FDA-approved drugs specifically for RBD. But two medications are used off-label with strong real-world results: melatonin and clonazepam.
Melatonin is a natural hormone your body makes to regulate sleep. In RBD, it’s used in much higher doses than for jet lag-typically starting at 3 mg at bedtime and increasing by 3 mg every 2-4 weeks up to 12 mg. About 65% of patients see significant improvement. Side effects are mild: maybe a little morning grogginess, or a headache. One 68-year-old man reduced his weekly episodes from 7 to 1 after starting 6 mg nightly. He kept sleeping in the same bed with his wife-and she finally got a full night’s rest.
Clonazepam, a benzodiazepine, has been used for decades. It works by calming brain activity. Dosing starts low: 0.25-0.5 mg at bedtime. Most people respond within a week. Efficacy is high-80-90% of patients see fewer episodes. But it’s not without risks. About 22% report dizziness, 18% feel unsteady, and 15% feel overly sleepy during the day. For older adults, the risk of falls jumps by 34%. One patient stopped clonazepam after three months because she started falling twice a month. Her doctor switched her to melatonin.
Doctors now often start with melatonin, especially in older patients or those with balance issues. Clonazepam is still used when melatonin doesn’t work-or when symptoms are severe. But it’s not a long-term solution for everyone. Tolerance can develop, and withdrawal can trigger nightmares or agitation in 38% of people who quit cold turkey.

Other Medications: What Else Works?
Not everyone responds to melatonin or clonazepam. For those who don’t, doctors may try other options.
Pramipexole, a dopamine agonist used for Parkinson’s and restless legs syndrome, helps about 60% of RBD patients-especially those who also have leg restlessness. Dose is low: 0.125-0.5 mg daily. It’s not a first choice, but it can be useful in combination.
Rivastigmine, a cholinesterase inhibitor used in dementia, showed promise in one small study for RBD patients with mild memory problems who didn’t respond to other treatments. It’s not widely used yet, but it’s an option for those with cognitive changes.
The most exciting new direction? Dual orexin receptor antagonists. Orexin is a brain chemical that helps keep you awake. Blocking it may help restore normal muscle control during REM sleep. Mount Sinai research in October 2023 showed a 78% drop in dream enactment behaviors in animal models. Suvorexant (Belsomra), already approved for insomnia, is being tested in humans for RBD. Neurocrine Biosciences’ drug NBI-1117568 received Fast Track status from the FDA in January 2023-meaning it could be available in the next few years.
Safety First: Modifying Your Bedroom
Medication helps-but it’s not enough. About 78% of people with RBD make safety changes at home. Why? Because even with treatment, episodes can still happen.
Here’s what works:
- Remove all weapons from the bedroom-guns, knives, tools.
- Pad sharp corners of furniture with foam or pillows.
- Place thick rugs or mats next to the bed to cushion falls.
- Install bed rails or use a low bed frame.
- Consider sleeping in separate beds if episodes are violent or frequent.
One study found 42% of patients eventually sleep apart from their partners-not because they want to, but because they’re afraid of hurting them. That’s heartbreaking. But it’s better than a broken bone or a trip to the ER.
What to Avoid
Alcohol is a major trigger. Even one or two drinks can double the risk of an RBD episode. Studies show 65% of patients have worse symptoms after drinking. So if you have RBD, skip the nightcap.
Also avoid certain medications: antidepressants (especially SSRIs and SNRIs), some sleep aids, and stimulants can worsen RBD. Always tell your doctor you have RBD before starting any new drug.
Neurological Monitoring: Watching for the Next Step
Because RBD is often a warning sign, regular neurological checkups are essential. The American Academy of Neurology recommends annual exams for anyone with idiopathic RBD.
What are they looking for? Early signs of Parkinson’s: slight tremors, reduced arm swing when walking, soft speech, or trouble with fine motor tasks like buttoning a shirt. Changes in smell, constipation, or REM sleep changes can also appear years before motor symptoms.
Annual assessments aren’t about panic-they’re about early intervention. If Parkinson’s is caught early, treatments can slow progression and improve quality of life. That’s why RBD is no longer just a sleep problem. It’s a neurological red flag.
What’s Next for RBD Treatment?
The field is moving fast. The global RBD market is expected to hit $1.2 billion by 2023 and grow 5.7% yearly through 2030. Why? Because more people are being diagnosed-and because researchers are finally focusing on the root cause.
Right now, all treatments manage symptoms. But the real goal is to stop the brain degeneration before it starts. Clinical trials are underway to test drugs that might delay or prevent Parkinson’s in RBD patients. The hope is that within five years, we’ll have the first disease-modifying therapies-not just symptom blockers.
For now, the best approach is simple: get diagnosed, treat the symptoms, make your bedroom safe, and stay on top of your neurological health. You’re not just sleeping better-you’re protecting your future brain.
Can REM sleep behavior disorder be cured?
There’s no cure for RBD yet. But medications like melatonin and clonazepam can reduce symptoms in most people. The bigger goal is to monitor for underlying neurodegenerative diseases like Parkinson’s, where early treatment can make a major difference in long-term outcomes.
Is melatonin safe for long-term use in RBD?
Yes. Melatonin is one of the safest options for long-term use in RBD. Side effects are rare and mild-mostly drowsiness or headaches. Unlike clonazepam, it doesn’t cause dependence, tolerance, or balance problems. Most people can take 6-12 mg nightly for years without issues.
Why is clonazepam risky for older adults with RBD?
Clonazepam can cause dizziness, unsteadiness, and daytime sleepiness-side effects that increase fall risk by 34% in people over 65. Falls in older adults can lead to fractures, hospitalization, or even death. For this reason, many doctors avoid clonazepam in elderly patients unless melatonin fails and symptoms are severe.
Can alcohol make RBD worse?
Yes. Even one or two drinks can trigger RBD episodes in 65% of patients. Alcohol disrupts the normal brain signals that keep muscles still during REM sleep. Avoiding alcohol is one of the most effective non-medication ways to reduce episodes.
Should I get a sleep study if my partner says I act out my dreams?
Absolutely. If your partner reports you yelling, punching, kicking, or jumping out of bed during sleep, you should see a sleep specialist. Polysomnography is the only way to confirm RBD-and early diagnosis can prevent injury and help detect neurodegenerative diseases before they progress.
How often should I see a neurologist if I have RBD?
Annual neurological exams are recommended. RBD has a 6.3% annual chance of progressing to Parkinson’s, dementia with Lewy bodies, or another neurodegenerative disease. Regular checkups help catch early signs like subtle movement changes, loss of smell, or constipation-signs that can appear years before full-blown symptoms.


Lynsey Tyson
December 21, 2025 AT 08:03Also, we got rid of all the sharp furniture. Just put foam padding on the bed frame. Small changes, huge difference.
Edington Renwick
December 22, 2025 AT 20:31Aboobakar Muhammedali
December 23, 2025 AT 08:46my dad had this and no one knew until he broke his hip falling out of bed. we were so scared. he took melatonin for 5 years and never had a fall again. he passed last year from parkinson's but at least he didn't hurt himself before that. thank you for writing this. people need to know.
Laura Hamill
December 24, 2025 AT 20:17They don't want you to know that 5G towers are triggering this disorder so they can push brain implants later. That's why they only approve melatonin and clonazepam-because they're cheap and easy to control. The real cure is a frequency blocker and a copper hat. I tried it. My husband stopped yelling. The doctors are furious.
pascal pantel
December 25, 2025 AT 00:02Gloria Parraz
December 25, 2025 AT 02:02You’re not alone. There’s help. And yes, it gets better.
Sahil jassy
December 26, 2025 AT 01:44Doctors need to stop pushing benzos on old folks. Melatonin is the real MVP.
Kathryn Featherstone
December 26, 2025 AT 08:05And yes, melatonin is safe long-term. I’ve had patients on it for 8 years. No issues.
Nicole Rutherford
December 27, 2025 AT 00:51Nancy Kou
December 28, 2025 AT 12:45Hussien SLeiman
December 29, 2025 AT 08:15Carolyn Benson
December 30, 2025 AT 03:06William Liu
December 30, 2025 AT 20:13