Myxedema coma isn’t just a rare complication of hypothyroidism-it’s a ticking clock. When your body runs out of thyroid hormone, everything slows down: your heart, your breathing, your brain. And when it hits critical, you don’t just feel tired-you stop responding. This isn’t a slow decline. It’s a medical emergency that kills 25% to 60% of people who don’t get help fast enough. Even worse, many patients are misdiagnosed for months, their symptoms written off as aging, depression, or just being "lazy." But the signs are there-if you know what to look for.
What Really Happens in Myxedema Coma?
Myxedema coma, now more accurately called myxedema crisis, happens when thyroid hormone levels crash. Your body depends on T3 and T4 to keep your metabolism running. Without them, your cells can’t produce energy. Your body temperature drops below 95°F (35°C). Your heart rate slows to under 60 beats per minute. Your breathing becomes shallow-sometimes fewer than 12 breaths per minute. Your brain fogs over. You might not even recognize your own family.
This isn’t theoretical. In 80-90% of cases, patients are hypothermic. In 98%, they’re profoundly lethargic. Nearly 8 out of 10 have hyponatremia-dangerously low sodium. And most of them have had untreated or poorly managed hypothyroidism for years. It’s not sudden. It’s the slow burn of neglect that finally explodes.
What makes it deadly isn’t just the low hormones. It’s what follows: respiratory failure, heart rhythm problems, kidney shutdown, and intestinal paralysis. Up to 60% of patients develop ileus-their gut stops moving. Constipation turns into megacolon. Fluid builds up in the skin, especially around the eyes and face. That’s the "myxedema" part-the thick, swollen, non-pitting edema that gives the condition its name.
Who’s at Risk?
Most patients are women over 60. The female-to-male ratio is about 3:1. But here’s the hidden danger: men and younger people get it too-and they’re more likely to be missed. Healthline’s patient data shows men account for only 25% of cases but 40% of diagnostic delays. Why? Because doctors don’t expect it. A 45-year-old man with fatigue and cold intolerance? He’s told to "get more sleep." A 55-year-old woman with memory issues? "Just perimenopause."
Winter is the worst season. Cold exposure is a trigger in nearly one-third of cases. A patient who forgets to take their thyroid pill during a hospital stay for pneumonia? That’s a classic setup. Infections-especially pneumonia and UTIs-are the number one precipitating factor, responsible for 30-50% of crises. Other triggers include heart attacks, strokes, certain medications (like sedatives or lithium), and sudden withdrawal from thyroid hormone.
And it’s not just about access to care. Uninsured patients wait 35% longer for treatment and have 22% higher death rates. This isn’t just a medical problem-it’s a systemic one.
How Is It Diagnosed?
There’s no single lab test that confirms myxedema coma. That’s why so many cases are missed. You don’t wait for results-you act on suspicion.
The diagnostic triad is simple: altered mental status, hypothermia, and a triggering event. But symptoms can be subtle. Elderly patients often show "apathetic hypothyroidism"-no tremors, no weight gain, no dry skin. Just confusion, low energy, and a strange refusal to get out of bed. One patient on the American Thyroid Association forum described it as "feeling like I was moving through molasses." That’s not depression. That’s your brain starving for hormone.
Lab findings usually show:
- TSH >10 mIU/L (often over 100)
- Free T4 < 0.9 ng/dL
- Sodium < 135 mmol/L
- PaO2 < 80 mmHg, PaCO2 > 45 mmHg (signs of respiratory failure)
- Low glucose, low cortisol (due to impaired adrenal response)
But here’s the key: you don’t wait for these results. If a 72-year-old woman with known hypothyroidism is found unresponsive and cold, you start treatment before the blood comes back.
Emergency Protocol: What to Do Immediately
Time kills. Every hour of delay increases mortality by 10%. The goal is simple: restore thyroid hormone and support failing organs-right now.
Step 1: Secure the airway
Half to 70% of patients need intubation. Their breathing is too slow. Their cough reflex is gone. They can’t protect their lungs. Don’t wait for oxygen saturation to drop. If they’re lethargic and breathing shallowly, intubate.
Step 2: Give thyroid hormone-immediately
Start with intravenous levothyroxine (T4): 300-500 mcg as a loading dose. Then 50-100 mcg daily. For patients with heart disease or severe shock, add liothyronine (T3): 10-20 mcg every 8 hours. The 2022 Endocrine Society update says T3 should be first-line in cardiac compromise. Why? Because T3 acts faster. T4 takes days to convert. In crisis, you don’t have days.
Step 3: Rewarm slowly
No heating blankets. No warm baths. Active warming can cause dangerous drops in blood pressure as blood vessels dilate before the body can handle the increased metabolic demand. Use warm blankets, heated rooms, and monitor core temperature every 30 minutes. Let the body warm up on its own-once the hormone is in.
Step 4: Treat the trigger
Assume infection until proven otherwise. Start broad-spectrum antibiotics-cover pneumonia, UTI, and sepsis. Don’t wait for cultures. Infection is the trigger in nearly half of all cases.
Step 5: Correct electrolytes carefully
Hyponatremia is common, but correcting sodium too fast can cause brain damage. Limit correction to 4-6 mmol/L in the first 24 hours. Use fluids cautiously. Many patients are volume-depleted, but some have dilutional hyponatremia from low ADH. Give saline only if needed, and monitor closely.
Use the DIMES mnemonic to remember triggers: Drugs, Infection, Myocardial infarction/CVA, Exposure to cold, Stroke.
Why Do So Many People Die?
It’s not the disease. It’s the delay.
On average, patients wait 6-12 hours before getting treatment. That’s because the symptoms look like other things: stroke, sepsis, drug overdose, dementia. And because many patients have been undiagnosed for years, their doctors don’t suspect hypothyroidism.
One case report describes a 68-year-old woman who was misdiagnosed with depression for 18 months. She stopped her thyroid medication during a hospital stay for pneumonia. Three days later, she was found unconscious. She spent 11 days in the ICU. She survived-but barely.
Another patient on Reddit said, "I wore three layers inside a 75°F room and still shook. No one believed me."
When treatment starts early, recovery is dramatic. Many patients wake up within 24-48 hours. Their heart rate normalizes. Their temperature rises. Their confusion lifts. But if you wait? The brain doesn’t recover as well. The heart weakens. The kidneys fail. The chance of survival drops fast.

What’s Changing in Treatment?
Things are improving. In January 2023, the FDA approved a new IV thyroid hormone formulation called Thyrogen® with faster absorption. That means quicker hormone delivery when every minute counts.
Research is also moving toward early detection. A 2023 Lancet study found that elevated thyrotropin receptor antibody levels predict decompensation with 85% sensitivity. That could lead to screening for high-risk patients before they crash.
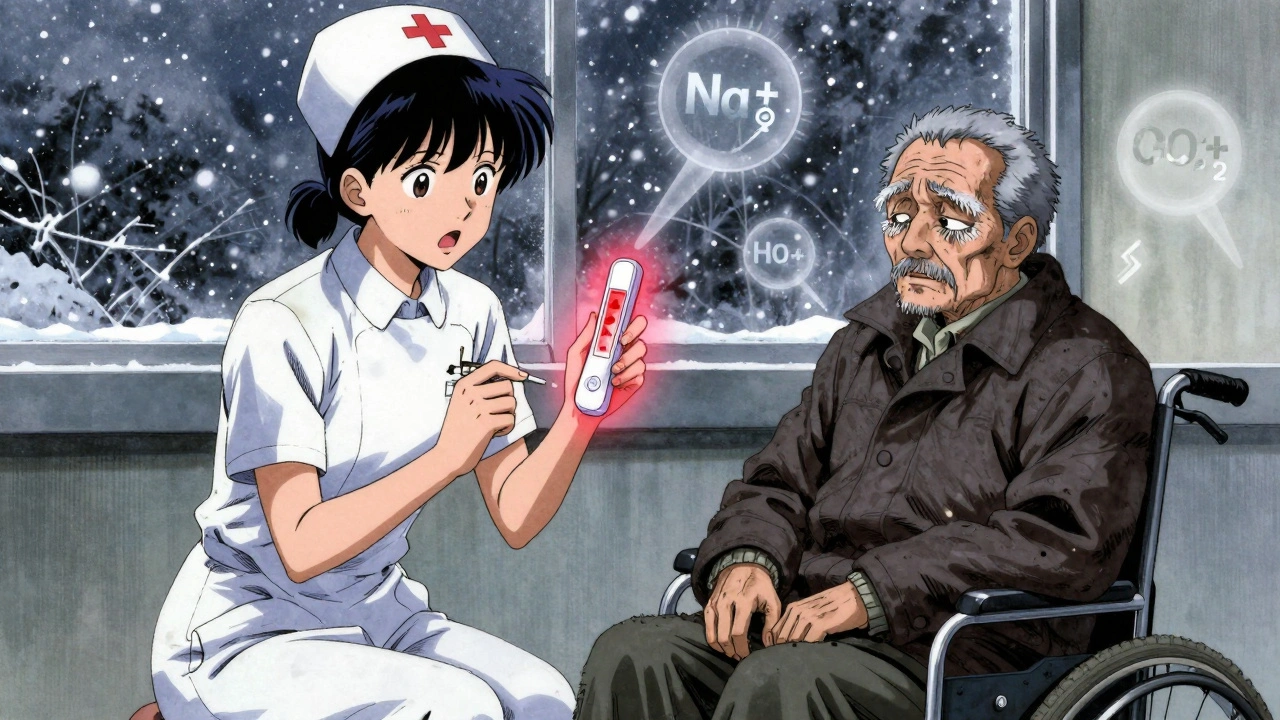
Point-of-care thyroid testing is in phase 3 trials. These devices can give results in 15 minutes-instead of hours. Imagine an ER nurse running a quick test on a confused elderly patient and getting TSH and T4 levels before the doctor even walks in.
But the biggest change? The mindset. Doctors are learning: don’t wait for labs. If the clinical picture fits, treat.
What Happens After?
Survivors need lifelong thyroid hormone replacement. They need regular monitoring. And they need education-because many don’t realize how fragile their balance is. Missing one dose during an illness can be deadly.
Patients who’ve been through it say the same thing: "Take your pills. Even when you feel fine. Even when you’re sick. Even if you think it’s just a cold."
And for caregivers: if someone with hypothyroidism suddenly becomes confused, cold, or unresponsive-call 911. Don’t wait. Don’t assume it’s "just old age." Myxedema coma doesn’t announce itself. It creeps in. And if you act fast, you can save a life.
Can myxedema coma happen to someone who’s taking thyroid medication?
Yes. Even patients on medication can develop myxedema coma if they miss doses, especially during illness, surgery, or extreme cold. Stopping thyroid hormone abruptly-even for a few days-can trigger a crisis. Infections, hospitalizations, and certain drugs (like lithium or amiodarone) can also interfere with hormone absorption or function. Never stop thyroid medication without medical supervision.
Is myxedema coma the same as thyroid storm?
No. They’re opposites. Myxedema coma is caused by too little thyroid hormone; thyroid storm is caused by too much. Thyroid storm brings high fever, rapid heartbeat, agitation, and vomiting. Myxedema coma brings low temperature, slow heart rate, lethargy, and coma. Treatment is completely different: thyroid storm uses drugs to block hormone production; myxedema coma needs immediate hormone replacement. Confusing the two can be fatal.
Why is rewarming so dangerous in myxedema coma?
Active rewarming (like heating blankets or warm IV fluids) can cause sudden blood vessel dilation, leading to a sharp drop in blood pressure. But your body can’t respond because it lacks thyroid hormone to increase metabolism and heart function. This can trigger cardiac arrest. Passive rewarming-warm blankets, room temperature-lets the body warm slowly as hormone levels rise. Only after hormone replacement should you consider gentle active warming.
Can you prevent myxedema coma?
Yes, in most cases. Regular thyroid hormone replacement and annual TSH checks are key. Patients should carry a medical alert card and know to increase their dose during illness (under doctor guidance). Avoid cold exposure if you’re elderly or have known hypothyroidism. If you’re hospitalized, make sure your thyroid medication is restarted immediately. And if you’re a caregiver-watch for sudden confusion, extreme cold, or unresponsiveness. Early action saves lives.
Why is hyponatremia so common in myxedema coma?
Low thyroid hormone reduces kidney function and impairs the body’s ability to excrete free water. This leads to water retention and diluted sodium levels. It’s not caused by dehydration-it’s caused by your kidneys not working properly. Correcting sodium too quickly can damage the brain, so it must be done slowly-no more than 4-6 mmol/L in 24 hours. Always check sodium levels in any hypothyroid patient who seems confused or lethargic.


Jimmy Kärnfeldt
December 10, 2025 AT 17:03Man, this hit different. I had an aunt who went through something like this-doctors kept saying it was depression, then dementia. She was just cold and quiet, didn’t eat, didn’t talk. We didn’t know until she collapsed. If this post saves even one life, it’s worth every word.
Aman deep
December 11, 2025 AT 01:21bro i live in india and we dont even have easy access to thyroid tests in small towns. my uncle missed his meds for 3 days after a fever and ended up in icu for 2 weeks. nobody thought it was thyroid. they thought he was just old. 😔
Vivian Amadi
December 11, 2025 AT 11:29Stop pretending this is rare. It’s a systemic failure. Hospitals ignore hypothyroid patients because they’re old, poor, or female. This isn’t medicine-it’s classism with a stethoscope.
Eddie Bennett
December 11, 2025 AT 22:07I’m not a doc but I’ve seen this play out twice. The rewarming thing blew my mind. I always thought you’d want to warm someone up ASAP. Turns out you gotta let the hormones do the work first. Wild how much we assume we know.
Ariel Nichole
December 13, 2025 AT 09:31Thanks for writing this. My mom’s been on levothyroxine for 15 years and I’ve been nagging her to never skip doses. Now I’ve got real data to back it up. She’s gonna read this.
Taylor Dressler
December 13, 2025 AT 18:49Correction: The 2022 Endocrine Society guidelines recommend T3 as an adjunct in cardiac compromise, not first-line. T4 remains primary. T3 is reserved for patients with hemodynamic instability or when rapid effect is critical. Precision matters in emergencies.
Aidan Stacey
December 15, 2025 AT 17:02My sister’s a nurse in a rural ER. She told me about a guy who came in with ‘flu symptoms’-38, male, no history. She noticed his skin was puffy, he was shivering in a t-shirt, and his pulse was 48. She ordered a TSH on instinct. He was in myxedema crisis. Saved by a nurse who didn’t buy the ‘just tired’ story. These are the heroes.
Courtney Blake
December 16, 2025 AT 22:02Oh great, another guilt-trip article. People who don’t take their meds deserve what they get. Stop coddling noncompliant patients. Also, why is this in English? I’m not American.
Lisa Stringfellow
December 18, 2025 AT 16:56So… this is just a fancy way of saying ‘take your pills’? I mean, really? 2000 words to tell people to not skip levothyroxine? The fact that this even needs explaining is depressing.
Kristi Pope
December 19, 2025 AT 00:09My grandma used to say ‘thyroid’s like a battery-you gotta charge it daily’ and she was right. She survived this twice. Took her 6 months to walk again after the first one. She still takes her pill at 8am sharp, rain or shine. I’m printing this out for her doctor.
Sylvia Frenzel
December 20, 2025 AT 20:22Why are we wasting time on this? We’ve got real emergencies. Gun violence, inflation, climate collapse. This is just a niche condition for old ladies. Fix the system, not the symptoms.
Paul Dixon
December 21, 2025 AT 16:49my cousin’s a med student and she told me they don’t even teach this well in med school. they rush through endo because it’s ‘boring.’ so doctors miss it because they were never trained to see it. that’s the real problem.
matthew dendle
December 23, 2025 AT 09:29so if i dont take my pill and i get pneumonia i just die? wow thanks for the update. maybe i shoulda stayed on the couch like the doc said
Monica Evan
December 24, 2025 AT 07:06as a nurse from a rural clinic in texas, i’ve seen this too many times. patients come in with sodium at 120, temp at 92, and no one connects it. we don’t have fancy point-of-care tests yet. we just pray they’re on meds. this post? it’s a lifeline for people like me who fight daily just to be heard.
Jimmy Kärnfeldt
December 25, 2025 AT 17:31Just read the last comment from Monica. That’s why I’m here. Real people, real stories, real stakes. Not just data. That’s what makes this matter.