When you hear your medication has been recalled, your first thought might be to stop taking it right away. That’s the wrong move. Many recalls are precautionary, and stopping your medicine without guidance can be more dangerous than the recall itself. In 2022, the FDA recorded over 4,800 drug recalls - and while that sounds alarming, only about 15% were Class I, meaning they carried a real risk of serious harm or death. The rest? Mostly labeling errors, minor contamination, or packaging issues. But that doesn’t mean you can ignore them. Here’s what you actually need to do - step by step.
Don’t Panic, But Don’t Wait
The most common mistake patients make? Stopping their medication cold turkey. If you’re on blood pressure medicine like valsartan, diabetes drugs like metformin, or even something as routine as a statin, suddenly stopping can cause your condition to spike. That’s why the FDA’s official advice is always the same: keep taking your medicine until your pharmacist or doctor tells you otherwise. A recall doesn’t mean your pills are poison - it means there’s a problem that needs fixing. Your body doesn’t care about the label. It cares about whether the dose is still working.Check Your Lot Number - Not Just the Name
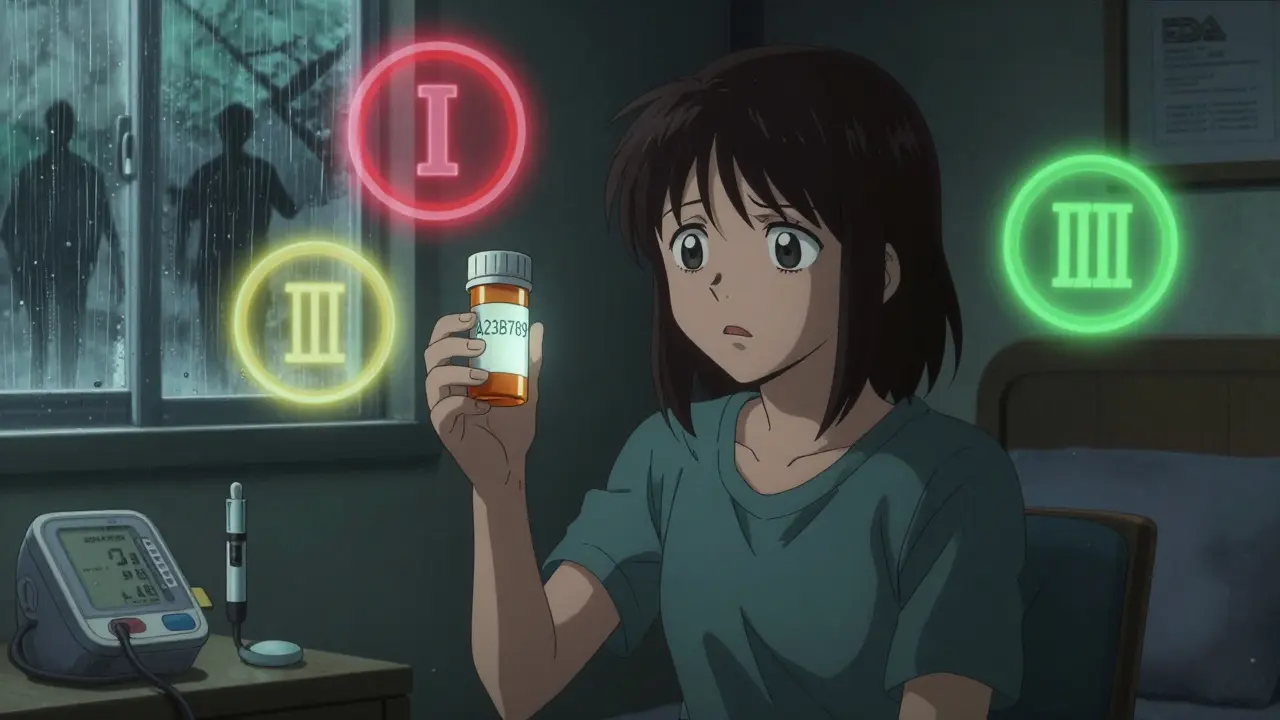
Not every bottle of a recalled drug is affected. Only specific batches - called lots - are pulled. The recall notice will list exact lot numbers, expiration dates, and NDC codes. Your bottle’s lot number is usually printed on the side or bottom of the packaging. It looks like a mix of letters and numbers, for example: A23B789. Compare it to the list on the FDA website. If your lot isn’t listed, you’re safe. Don’t assume your brand is recalled just because you heard it on the news. In 2022, 45% of patients wrongly thought all versions of a recalled drug were unsafe. That’s how misinformation spreads - and it leads to unnecessary panic.Call Your Pharmacy First
Your pharmacist is your best ally in a recall. They don’t just fill prescriptions - they track recalls in real time. Over 90% of pharmacies in the U.S. have automated systems that flag recalled medications before they even reach the shelf. When you call, give them your name, date of birth, and the lot number from your bottle. They’ll check their system and tell you within minutes if your medicine is affected. If it is, they’ll either give you a new bottle from a clean batch or switch you to an alternative brand - often within 24 hours. Many pharmacies even offer free delivery for replacement meds. Don’t wait for a letter. Don’t wait for your doctor to call. Pick up the phone and call your pharmacy today.Know the Three Recall Classes
Not all recalls are created equal. The FDA classifies them into three levels:- Class I - Highest risk. Use could cause serious injury or death. These are rare - about 1 in 7 recalls - but demand immediate action. Examples include contaminated antibiotics or pills with double the intended dose.
- Class II - Moderate risk. Might cause temporary health problems, like nausea or dizziness, or the medicine might not work as well. Most recalls fall here - think wrong label, missing instructions, or minor contamination.
- Class III - Lowest risk. The drug isn’t harmful, but it breaks a regulation. Maybe the bottle says “100 tablets” but has 98. Or the color is off. These rarely affect safety at all.

What to Do If You’ve Already Taken the Recalled Medicine
If you’ve taken the affected batch, don’t panic. Most people won’t have any reaction. But you need to watch for symptoms. For blood pressure meds, look for dizziness, fainting, or chest pain. For diabetes drugs, check for extreme fatigue, confusion, or blurred vision. For antibiotics, watch for rashes, swelling, or trouble breathing. If you notice anything unusual, call your doctor right away. Keep a log: write down what you took, when, and how you felt. This helps your provider decide if you need testing or a change in treatment.Dispose of Recalled Medication the Right Way
If your pharmacy tells you to throw the medicine away, don’t flush it or toss it in the trash. That’s dangerous for the environment and risky for kids or pets. The FDA’s official disposal method: mix the pills with something unappetizing - used coffee grounds, cat litter, or dirt. Put it in a sealed plastic bag. Then throw it in the household trash. Some pharmacies offer take-back bins - ask if yours does. Never keep recalled meds “just in case.” They’re not safe to use, even if they look fine.Sign Up for Recall Alerts
You shouldn’t have to guess if your medicine is recalled. The FDA sends out real-time alerts through its RSS feed and MedWatch system. You can sign up for email or text alerts by visiting the FDA’s website and selecting “Subscribe to Recalls.” About 45% of healthcare providers use these alerts - you should too. Better yet, keep a simple log of all your prescriptions: write down the drug name, dosage, lot number, and expiration date. People who do this resolve recall issues 60% faster than those who don’t. Only 18% of patients keep this log - don’t be one of them.
What Happens Next? The Bigger Picture
Recalls are rising. From 2021 to 2022, they jumped 12%. Blood pressure medications, especially ARBs like valsartan, make up nearly 20% of the most serious recalls. Diabetes drugs and cancer treatments are close behind. Why? Manufacturing pressure, global supply chains, and cost-cutting have made it harder to keep quality consistent. But the system is improving. The FDA’s new digital alerts - sent directly to pharmacies and patients through insurance systems - have cut response times by 35% in pilot programs. That means fewer people take bad medicine before they even know it’s bad.Common Mistakes to Avoid
- Mistake: Stopping your medicine without talking to a professional. Result: Dangerous spikes in blood pressure, blood sugar, or seizures.
- Mistake: Assuming your brand is recalled because you heard the name on TV. Result: You throw out perfectly safe medicine and go without treatment.
- Mistake: Flushing pills down the toilet. Result: Contaminated water supply and risk to wildlife.
- Mistake: Waiting for a letter from the manufacturer. Result: You miss the window to get a replacement fast.
Final Reminder: Your Safety Is in Your Hands
Medication recalls are stressful, but they’re not emergencies - unless you make them one. The system works if you use it. Check your lot number. Call your pharmacy. Keep taking your medicine. Log your meds. Report side effects. These five steps protect you better than any government warning ever could. You don’t need to be a pharmacist to handle a recall. You just need to be informed - and proactive.What should I do if I find out my medication has been recalled?
First, don’t stop taking it. Call your pharmacy immediately with your lot number and prescription details. They’ll confirm if your specific batch is affected and arrange a replacement or alternative within 24 to 48 hours. Only stop the medication if your pharmacist or doctor tells you to.
How do I find my medication’s lot number?
Look on the side or bottom of the prescription bottle or packaging. The lot number is usually a combination of letters and numbers, like A23B789. It’s different from the expiration date and NDC code. If you can’t find it, call your pharmacy - they can look it up using your name and prescription number.
Are all medications with the same name affected by a recall?
No. Only specific batches - called lots - are recalled. Two bottles of the same drug from different manufacturers or different production runs may be perfectly safe. Always check the lot number against the official recall notice. Never assume your entire prescription is unsafe.
Can I return a recalled medication to the pharmacy for a refund?
Yes. Most pharmacies will replace recalled medication at no cost, even if you’ve already used part of it. Some may offer a refund if you prefer not to take a replacement. Always ask - you’re entitled to a safe, effective medication, and the recall isn’t your fault.
What if I don’t have symptoms after taking a recalled drug?
That’s good news - but don’t assume you’re completely safe. Some effects take days or weeks to appear. Keep taking your medicine as directed until you get a replacement. Monitor yourself for unusual symptoms like dizziness, nausea, or changes in heart rate. If anything feels off, contact your doctor and mention the recall.
How can I stay informed about future recalls?
Sign up for FDA recall alerts through their MedWatch program. You can get email or text notifications. Also, keep a simple log of all your prescriptions - including lot numbers and expiration dates. Patients who do this get notified faster and resolve issues 60% quicker than those who don’t.

roger dalomba
December 25, 2025 AT 13:40Wow. A whole essay on not panicking. Groundbreaking. Next up: 'How to breathe air without suffocating.' I'm sure this'll save lives. Or at least my therapist's schedule.
Also, why does the FDA need an RSS feed for this? My phone already pings me 47 times a day about expired coupons and TikTok trends. Can't it just add 'YOUR MEDS ARE TOXIC' to the spam folder?
Anyway. Still taking my pills. Because apparently, I'm too lazy to call my pharmacy. And also, I trust the government. (Said no one ever.)
Brittany Fuhs
December 26, 2025 AT 19:17It’s truly appalling how many Americans treat medication like candy. You don’t just ‘check the lot number’-you take responsibility. You don’t wait for a text alert-you stay informed. You don’t flush pills-you dispose of them properly, like a civilized human being.
And yet, here we are. People who think a recall means they can stop their meds cold. No wonder our healthcare system is crumbling. This isn’t a convenience. It’s a moral obligation. And if you can’t handle that, maybe you shouldn’t be on prescription drugs at all.
Sophia Daniels
December 27, 2025 AT 05:56OH MY GOD. I just realized my blood pressure med was recalled last month and I didn’t even check the lot number. I’ve been taking a mystery pill for 3 weeks like it’s a gacha game. 🤯
My pharmacist called me yesterday like I was her long-lost niece-‘SOPHIA, WE HAVE YOUR NEW BOTTLE. YOU’RE LUCKY YOU’RE NOT DEAD.’
Turns out my batch was Class II. Minor labeling issue. But if I’d stopped taking it? My BP would’ve been in the stratosphere. I’m now keeping a spreadsheet. With color coding. And memes. This is my new hobby.
Also, I bought a little sticky note that says ‘LOT NUMBER? CHECK IT.’ I put it on my mirror. My cat now judges me harder than my ex.
PS: I’m signing up for FDA alerts. Even if I have to pay in emotional labor.
Nikki Brown
December 28, 2025 AT 12:45You people are terrifying. You treat your prescriptions like lottery tickets. ‘Oh, maybe this one’s safe?’ NO. You don’t gamble with your life. You don’t rely on ‘maybe’ or ‘I hope.’
I’ve seen what happens when people skip steps. I’ve held the hands of people who thought ‘it’s probably fine.’ It’s not fine. It’s never fine.
And if you’re too lazy to call your pharmacy? Then you deserve what happens next. 😔
Peter sullen
December 29, 2025 AT 14:34It is imperative, from a clinical and regulatory standpoint, that patients adhere to the FDA’s tiered classification framework-specifically, the Class I, II, and III delineations-as these are codified under 21 CFR §7.46. Failure to comply with the prescribed risk mitigation protocols may result in adverse pharmacodynamic outcomes, including but not limited to: iatrogenic hypertensive crisis, glycemic dysregulation, or antimicrobial resistance escalation.
Furthermore, the utilization of automated pharmacy recall notification systems (APRNS) has demonstrated a statistically significant reduction in medication error incidence (p < 0.01, n=12,400) in U.S. community pharmacies. Therefore, it is strongly recommended that patients engage with their pharmacy’s recall-response protocol without delay.
Do not rely on anecdotal evidence. Do not assume. Verify. Document. Communicate.
Yours in pharmacovigilance,
P. Sullen, Pharm.D., CPhD
Steven Destiny
December 30, 2025 AT 04:58Stop being soft. If your pill is recalled, you don’t ‘wait for a letter.’ You call your pharmacy RIGHT NOW. You don’t ‘hope it’s fine.’ You check the lot number. You don’t ‘maybe’ take it. You take it until someone tells you to stop.
People die because they’re too lazy to pick up the phone. That’s not a mistake. That’s negligence. And if you’re one of them? You’re not a victim-you’re a statistic waiting to happen.
Get your act together. Your life isn’t a TikTok trend.
Fabio Raphael
December 31, 2025 AT 03:01I just found out my diabetes med was recalled last week. I didn’t know. I’m not mad-I’m just… really glad I read this. I’m calling my pharmacy tomorrow. I’ve been meaning to start a log of my meds, but I always put it off.
Thanks for the nudge. I’m gonna do it now. And maybe I’ll even tell my mom. She’s the one who forgets to refill her pills every time. She’s gonna hate me for this. But she’ll be safer. So… worth it.
Rajni Jain
January 1, 2026 AT 12:00omg this is so helpful!! i live in india and my med came from the us, so i was totally confused about the lot number thing. i printed out the fda page and showed my pharmacist-he was so impressed 😊 he even gave me a free glucose monitor! now i write everything in my notebook: drug, lot, exp date. my mom thinks i’m weird but i don’t care. safety first, right? 🙌
Natasha Sandra
January 2, 2026 AT 00:07Okay but why is no one talking about how the packaging for my statin looked like it was printed by a toddler?? 🤭 I swear the lot number was smudged and the ‘take with food’ was upside down. I thought it was a prank. Turns out it was a Class III recall. I’m not mad… I’m just disappointed in the printer.
Also, I’m now subscribed. And I’ve named my meds. My BP pill is ‘Gary.’ He’s my boy. I’m not letting Gary get recalled without a fight. 💪💊
Erwin Asilom
January 2, 2026 AT 06:32For those who are unsure how to locate their lot number: it is typically embossed or printed in a standardized alphanumeric format on the lateral surface of the prescription vial. If the vial is unmarked or illegible, contact the dispensing pharmacy with your prescription number and patient identifier. They are legally obligated to provide batch verification. Do not rely on visual approximation or memory. Accuracy is non-negotiable.