Every year, hundreds of thousands of people are harmed because of simple mistakes with their medications. Some take the wrong pill. Others take too much, too little, or at the wrong time. These aren’t rare accidents-they’re preventable. And they happen just as often at home as they do in hospitals.
In the U.S. alone, medication errors injure at least 1.5 million people annually. Globally, the World Health Organization estimates they cost $42 billion each year. The worst part? Nearly all of these errors could be stopped with better systems, better training, and better habits.
How Medication Errors Happen in Hospitals
Hospitals have more tools than ever to catch mistakes, but technology doesn’t fix everything. Barcode Medication Administration (BCMA) systems scan a patient’s wristband and the drug’s barcode before giving any medication. It sounds foolproof-and it works. One 2025 study in JMIR found BCMA cut dispensing errors by 44%. Wrong drug errors dropped by over half. Dose mistakes fell by 43%. Monitoring errors? Down 92%.
But here’s what nobody talks about: the beeping.
Nurses in a 500-bed hospital reported on Reddit that BCMA added 15-20 minutes to every medication round. The constant alerts, the scanning, the system slowdowns-it wears people down. Some nurses started bypassing the system just to keep up. A 2024 survey of 1,200 pharmacists found that while 68% saw fewer errors with BCMA, 57% admitted new errors had appeared because staff found workarounds.
Computerized Physician Order Entry (CPOE) systems help too. They stop doctors from prescribing dangerous combinations or wrong doses before the order even leaves their desk. Studies show CPOE cuts errors by at least 50%. But too many alerts? That’s a problem. Clinicians get so flooded with warnings that they start ignoring them. One study found 42% of doctors and nurses just click through alerts without reading them.
And then there’s medication reconciliation-the process of making sure a patient’s full list of meds is accurate when they move between units, or leave the hospital. It’s one of the most effective tools we have. But too often, it’s done poorly. A WHO report found that most hospitals get it wrong at discharge. Patients leave with a list that’s missing their blood pressure pills, or includes a drug they stopped taking months ago.
Why Home Medication Mistakes Are Just as Dangerous
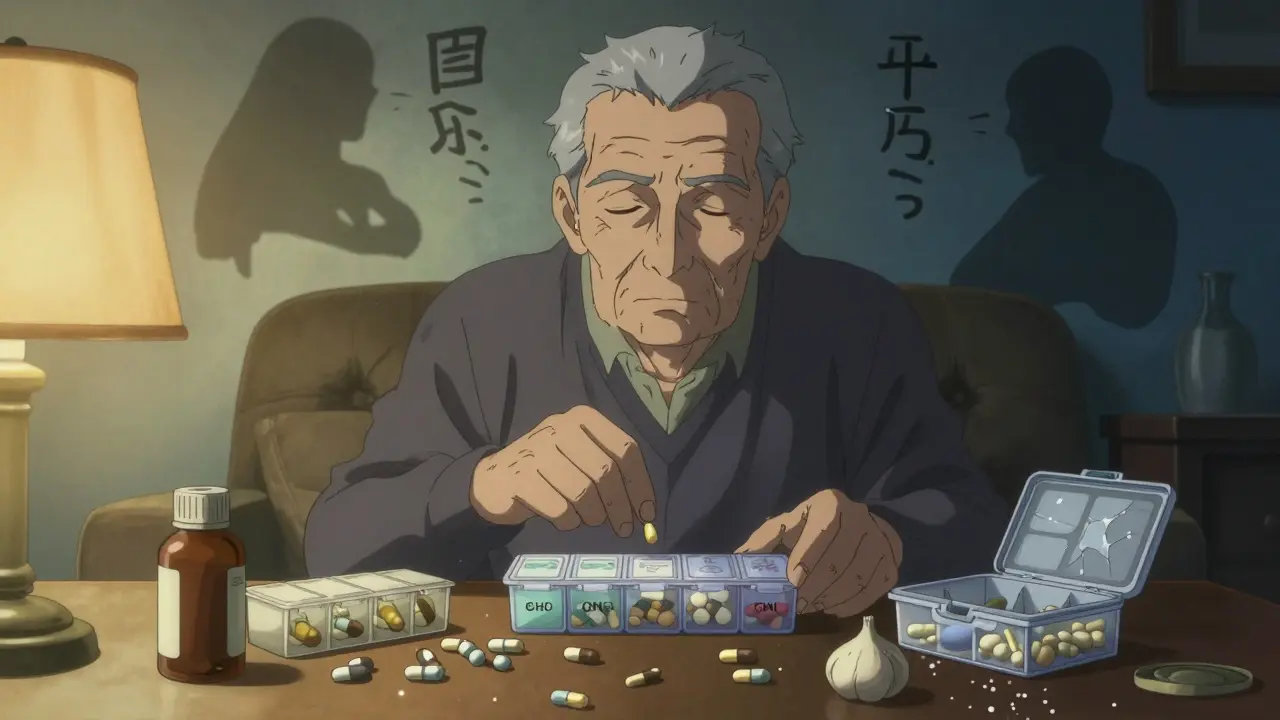
Most medication errors don’t happen in hospitals. They happen in kitchens, living rooms, and bedrooms. And the people most at risk? Seniors taking five or more pills a day.
A 2024 study in the Journal of Patient Safety found 89% of home medication errors involved people aged 75 or older. The biggest problem? Confusion. Not from memory loss-though that plays a role-but from too many containers, too many schedules, too many bottles.
Blister packs and pill organizers seem like the answer. But a 2025 review on SingleCare.com showed 72% of seniors using them still made at least one dosing error each month. Why? Because they used multiple organizers. One for morning, one for night, one for vitamins. Then they mixed them up. Sixty-three percent said they couldn’t tell which container held which drug.
Timing is another big issue. Forty-one percent of errors were because someone took their pill at 7 a.m. instead of 8 p.m. Thirty-three percent were wrong doses-half a pill instead of one, or two instead of one.
And don’t forget supplements. People don’t think of fish oil or vitamin D as “medications,” but they interact with prescriptions. A 78-year-old on blood thinners who starts taking garlic supplements without telling their doctor? That’s a recipe for bleeding.
What Actually Works to Stop These Mistakes
Technology helps-but only if it’s done right. BCMA works best when staff get real training. Not a 30-minute PowerPoint. Not a handout. Real, hands-on practice with simulated errors. One 2024 Johns Hopkins study found it took 3-6 months for nurses to get comfortable with BCMA. In the first month, error rates actually went up 12-15% as people struggled to adapt.
Successful hospitals don’t just install the system. They assign super-users-one for every 10 to 15 staff members-who answer questions, troubleshoot, and keep morale up. They hold biweekly feedback sessions. They link the system directly to the electronic health record so data flows smoothly.
At home, the solution is simpler but just as powerful: reduce complexity.
Patients taking five or more medications should aim for no more than three daily doses. If they need four pills in the morning, ask the pharmacist to combine them into one pill. Use single-dose packaging. A 2023 study in the Annals of Internal Medicine found that when pharmacists reviewed home meds weekly with elderly patients, errors dropped by 37%.
And don’t forget caregivers. A daughter who checks her mom’s pillbox every Sunday? That’s better than any app.
The Hidden Threat: Fake and Substandard Drugs
It’s not just about taking the wrong pill. Sometimes, the pill itself is fake.
The WHO warns that nearly all online pharmacies selling prescription drugs operate illegally. Many use fake Canadian logos, fake URLs with “canada” in them, and sell counterfeit insulin, blood pressure pills, or cancer drugs. These aren’t just ineffective-they’re deadly.
One patient in Ohio bought “generic” metformin from a website that looked official. The pills had no active ingredient. She ended up in the ER with diabetic ketoacidosis.
Experts like Dr. Marcus Schabacker of ECRI say we need to treat this like a public health emergency. The FDA and WHO are pushing for blockchain technology to track drug supply chains. In 2024, 12 U.S. health systems began testing blockchain to verify every pill from manufacturer to patient. It’s early, but it’s promising.
What You Can Do Right Now
Here’s what actually works-no tech required:
- Keep a written list of every medication, supplement, and over-the-counter drug you take. Include the dose and why you take it. Update it every time your doctor changes something.
- Use one pharmacy for all your prescriptions. That way, the pharmacist can catch interactions.
- Ask your pharmacist to put your meds in a single-dose blister pack. It’s often free or low-cost.
- Set phone alarms for each dose. Don’t rely on memory.
- Bring your list to every appointment-even if you think it’s “just a checkup.”
- Never take someone else’s pills, even if they have the same condition.
- Check online pharmacies with the FDA’s website. If it doesn’t require a prescription or looks sketchy, don’t buy from it.
What’s Next? AI and Better Systems
The future is coming. Johns Hopkins tested an AI tool in 2024 that predicted dangerous prescriptions before they were written. It cut high-risk errors by 53%. Hospitals are starting to use it.
But no algorithm will fix a nurse who’s rushed. No app will stop a patient from missing a dose because they’re confused.
Real progress comes from fixing systems-not just adding tech. It means training staff properly. It means simplifying regimens at home. It means listening to the people who use these systems every day.
Medication safety isn’t about perfection. It’s about reducing harm. And that starts with awareness, simple changes, and never assuming “it won’t happen to me.”

