What Is Immunotherapy for Allergies?
Immunotherapy isn’t just another allergy pill. It’s the only treatment that actually changes how your immune system reacts to allergens. Instead of masking symptoms like antihistamines do, it trains your body to stop overreacting to things like pollen, dust mites, or bee venom. This process is called desensitization. It’s been used since 1911, when two doctors in London first injected patients with small amounts of grass pollen to reduce their hay fever. Today, it’s backed by decades of research and is considered the gold standard for long-term allergy relief.
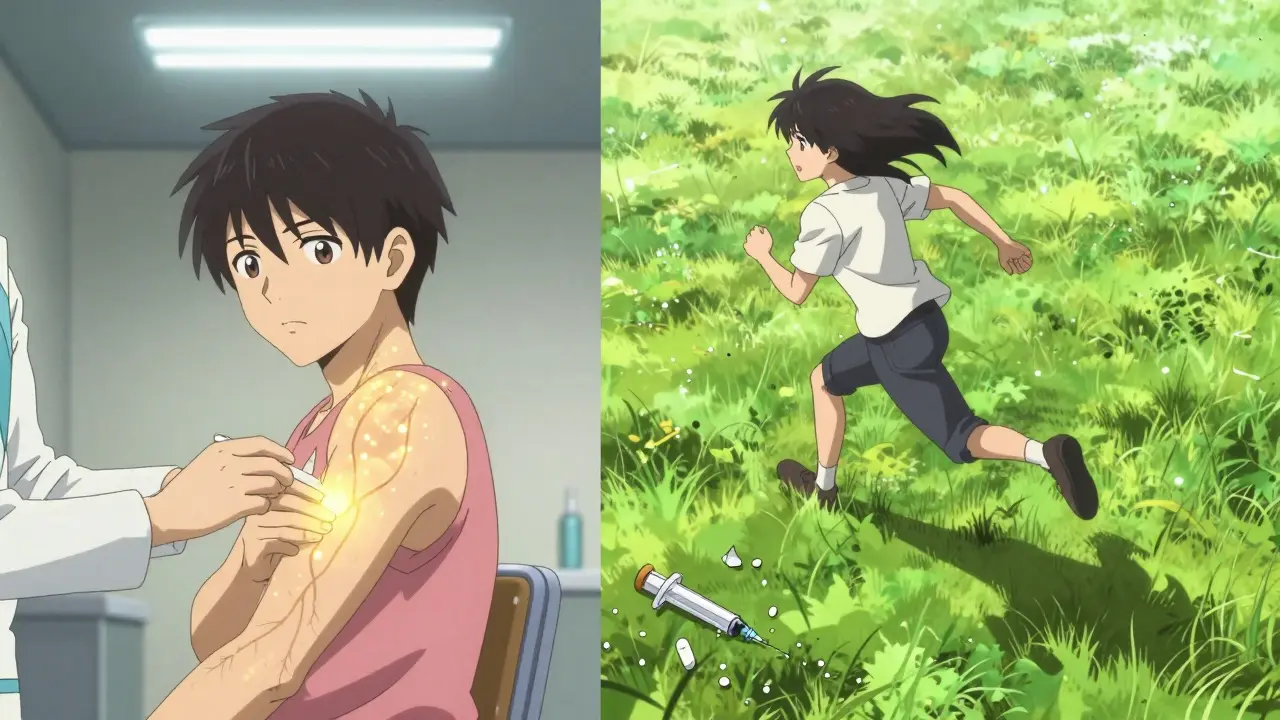
There are two main ways to do it: allergy shots (subcutaneous immunotherapy) and sublingual tablets. Both work by exposing you to tiny, controlled doses of the allergens you’re sensitive to. Over time, your immune system learns not to treat them as threats. The result? Fewer sneezes, less wheezing, and sometimes even a complete end to your allergy symptoms after 3 to 5 years of treatment.
Allergy Shots: The Proven Powerhouse
Allergy shots are the most effective form of immunotherapy. They’re custom-made for you based on your specific allergies. If you react to grass, ragweed, dust mites, and cat dander, your allergist can mix all four into one vial. That’s a big deal because nearly 8 out of 10 allergy sufferers are sensitive to more than one allergen. Single-allergen treatments just don’t cut it for most people.
The process has two phases. First, the build-up phase: you get shots once or twice a week for 3 to 12 months. Each shot contains a slightly higher dose of allergen until you reach the maintenance level. Then comes the maintenance phase-shots every 2 to 4 weeks for 3 to 5 years. Many clinics now offer cluster immunotherapy, which speeds up the build-up to just 4 to 9 weeks with 8 to 10 visits. Rush immunotherapy, used mostly for life-threatening insect sting allergies, gets you to maintenance in one 8-hour session.
Studies show 82% of people with multiple allergies see major symptom improvement with shots. A 2021 study in the Annals of Allergy, Asthma & Immunology found allergy shots reduced symptoms by 82%, compared to 67% for sublingual tablets. Patients who stick with it often report life-changing results. One Reddit user, after two years of ineffective tablets, switched to shots and cut their symptoms by 80%. That’s not rare-it’s common among those who complete the full course.
Sublingual Tablets: Convenience Without Compromise?
If you hate needles or can’t make weekly doctor visits, sublingual tablets are a solid alternative. These are small pills you place under your tongue every day. They’re FDA-approved for specific allergens: grass pollen (Oralair, Grastek), ragweed (Ragwitek), and dust mites (Odactra). Cat dander tablets (Cat-PAD) were approved in April 2024, expanding options.
The big advantage? No shots. No office visits. You take them at home, usually before breakfast. A 2022 survey found 92% of tablet users preferred this over weekly injections. For people who travel often, work irregular hours, or have kids with busy schedules, that convenience is priceless.
But there’s a catch. Each tablet covers only one allergen. If you’re allergic to both grass and dust mites, you’d need two different tablets. That’s expensive and hard to manage. And while they’re safe, they’re not as effective for complex cases. The same 2021 study showed tablets helped only 67% of patients with multiple allergies. On Healthgrades, 58% of negative reviews from tablet users mentioned they didn’t work well-often because they had more than one allergy.

Which One Is Right for You?
There’s no one-size-fits-all answer. Your choice depends on your allergies, lifestyle, and how much relief you need.
- Choose allergy shots if: You’re allergic to three or more allergens, your symptoms are severe, or you’ve tried medications without success. Shots offer the highest success rate and the best chance of long-term remission. They’re also the only option proven to prevent new allergies or asthma from developing.
- Choose sublingual tablets if: You’re allergic to just one allergen (like grass or dust mites), you can’t commit to weekly visits, or you’re needle-averse. They’re a good middle ground for mild-to-moderate cases where convenience matters more than maximum power.
Experts agree: if you have multiple allergies, shots are the clear winner. Dr. David M. Lang of Cleveland Clinic says, “Subcutaneous immunotherapy remains the most effective long-term treatment for allergic rhinitis.” Dr. Richard F. Lockey from USF Health puts it bluntly: “The requirement for separate tablets for each allergen makes comprehensive treatment impractical for most patients.”
What to Expect During Treatment
With allergy shots, you’ll spend time in the clinic during the build-up phase. Each visit takes about 30 minutes, including observation time after the injection. You might feel mild swelling or itching at the injection site-about 8.5% of people get local reactions. Systemic reactions (like hives or trouble breathing) are rare-only 2.1% with traditional build-up. Cluster and rush protocols have slightly higher risks, but clinics are trained to handle them.
With tablets, side effects are usually mild: an itchy mouth or throat, especially in the first few weeks. That’s normal. But if you get swelling of the tongue, trouble swallowing, or dizziness, stop taking it and call your doctor. You can’t just skip doses. If you miss more than 20% of your daily tablets, effectiveness drops to 45%. Setting phone reminders can boost adherence by 37%, according to a 2022 study.
Both treatments require patience. You won’t feel better right away. Most people notice improvements after 6 to 12 months. Full benefits take 2 to 3 years. And you can’t quit early-even if you feel fine. Stopping before 3 to 5 years means your immune system may forget what it learned.
Cost, Access, and Future Trends
Allergy shots cost more upfront because they require regular visits and custom allergen extracts. But insurance usually covers them. Sublingual tablets are pricier per month but have no office fees. The U.S. immunotherapy market is growing fast-projected to hit $2.94 billion by 2027. Shots still make up 68% of that market. Tablets are catching up, but only because they’re easier to use, not because they’re better.
Access is a real issue. There are only about 5,300 board-certified allergists in the U.S. Many rural areas have none. That’s why sublingual tablets are growing in popularity-they can be prescribed by any doctor, not just an allergist. But if you live near a good allergy clinic, shots are still the best bet.
The future looks promising. Multi-allergen sublingual tablets are in Phase 3 trials and could be available by 2025. Peptide-based therapies may cut treatment time from 5 years to just 2. And doctors are starting to use component-resolved diagnostics to tailor treatments even more precisely-knowing exactly which proteins in pollen or dust you react to.
Real Stories, Real Results
One woman in Bristol, who’s had hay fever since childhood, tried antihistamines for 15 years. They helped a little, but she still couldn’t run outside or open windows in spring. After switching to allergy shots, her symptoms dropped by 85% in two years. She now walks her dog without sneezing. “I didn’t think I’d ever feel normal again,” she said.
A man in Manchester, a truck driver with dust mite allergies, couldn’t stick with weekly shots. He switched to Odactra tablets. He takes them every morning before leaving home. “It’s not perfect,” he says, “but I don’t wake up choking on mucus anymore. That’s enough.”
These aren’t outliers. They’re the norm. The people who succeed with immunotherapy aren’t the ones who want the easiest option-they’re the ones who stick with the one that works.
Is Immunotherapy Worth It?
If you’ve spent years buying tissues, popping pills, and avoiding pollen season like a plague, then yes. Immunotherapy isn’t quick. It’s not flashy. But it’s the only treatment that can give you back your life-not just for a few hours, but for decades.
It’s not for everyone. If your allergies are mild and you’re okay with managing them, maybe skip it. But if you’re tired of symptoms controlling your life, immunotherapy is the closest thing to a cure we have today. Talk to an allergist. Get tested. Don’t assume tablets are the only easy way out. For most people, shots are still the answer.


Lance Nickie
January 15, 2026 AT 07:01Acacia Hendrix
January 15, 2026 AT 14:22Milla Masliy
January 16, 2026 AT 12:29Avneet Singh
January 17, 2026 AT 22:16Adam Vella
January 18, 2026 AT 21:33vishnu priyanka
January 19, 2026 AT 13:11Diana Campos Ortiz
January 21, 2026 AT 05:51Jesse Ibarra
January 21, 2026 AT 16:36jefferson fernandes
January 22, 2026 AT 17:50James Castner
January 23, 2026 AT 11:02Adam Rivera
January 25, 2026 AT 03:45Rosalee Vanness
January 25, 2026 AT 15:03lucy cooke
January 27, 2026 AT 05:01Trevor Davis
January 28, 2026 AT 18:52