Switching from brand-name immunosuppressants to generics can save hundreds of dollars a month - but for transplant patients, that savings might come with a hidden risk. Cyclosporine and tacrolimus aren’t like regular pills. They’re narrow therapeutic index (NTI) drugs, meaning the difference between a dose that works and one that causes rejection or toxicity is razor-thin. When generics are swapped in, even small changes in how the body absorbs the drug can trigger serious problems.
Why These Drugs Are Different
Both cyclosporine and tacrolimus stop your immune system from attacking a transplanted organ. They do this by blocking calcineurin, a protein that tells T-cells to fight. But that’s where the similarity ends. Tacrolimus is about 20 to 100 times more potent than cyclosporine. You take 5 mg of tacrolimus twice a day - but 150 mg of cyclosporine. Their blood targets are miles apart too: tacrolimus levels should stay between 5-15 ng/mL, while cyclosporine needs to be between 100-200 ng/mL in the first few months after transplant.Even tiny changes in how your body absorbs these drugs can push levels outside the safe range. That’s why both drugs require frequent blood tests - sometimes weekly after a switch. A drop from 8.5 to 5.2 ng/mL in tacrolimus, as one transplant patient reported, led to a rejection episode. That’s not rare. Studies show 18% of patients switching to generic tacrolimus need dose adjustments within weeks.
Generic Versions: Same Drug, Different Results
There are over 14 FDA-approved generic versions of tacrolimus and 11 of cyclosporine. They all meet the FDA’s bioequivalence standard: their absorption must fall within 80-125% of the brand-name drug. Sounds fair, right? But here’s the catch: that range is huge. A 25% difference in absorption can mean the difference between rejection and overdose.For cyclosporine, the problem is worse. Older versions used oil-based formulas that absorbed unpredictably. Even the newer microemulsion version (Neoral) has variability between manufacturers. One generic might dissolve faster than another, leading to higher peak levels. Another might absorb slower, causing levels to drop below the threshold needed to prevent rejection.
Transplant centers have seen this play out. One patient switched from brand Prograf to a generic tacrolimus made by Company A. Levels stayed stable. Then, because of insurance rules, they were switched to a different generic from Company B. Within two weeks, levels plunged. They ended up hospitalized. This isn’t anecdotal - it’s documented in clinical studies and patient forums.
Real Stories, Real Consequences
On Reddit’s r/transplant community, dozens of patients describe the same pattern: stable for months, then a switch, then panic. One user wrote, “I was doing great on Prograf. Insurance forced me to generic. My levels dropped. My creatinine spiked. I had a biopsy - it showed rejection.” Another said, “My nephrologist won’t let me switch to generic cyclosporine. The first one we tried made me dizzy and my levels swung like a pendulum.”But not everyone has bad experiences. Some patients report no issues after switching. One wrote, “I’ve been on generic tacrolimus for 18 months. Levels are perfect. Saved $900 a month.” The difference? Consistency. These patients stayed on the same generic brand. They didn’t get switched again.
Research backs this up. A 2022 survey of transplant centers found that 73% of them had to change their protocols when patients switched between different generic manufacturers. That’s because each new switch - even to another “approved” generic - can reset the risk clock.
Why Doctors Are Wary
Experts don’t oppose generics. They oppose random switching. Dr. BK Krämer, who led the landmark 2005 study comparing tacrolimus and cyclosporine, says: “Tacrolimus is clearly superior in preventing rejection. But switching between generics without monitoring? That’s dangerous.”The European Medicines Agency warned in 2020 that switching between generic tacrolimus products could cause “subtherapeutic or supratherapeutic concentrations.” The FDA’s own guidelines say bioequivalence studies are done in healthy volunteers - not transplant patients, whose bodies absorb drugs differently due to surgery, inflammation, and other meds.
Transplant pharmacists now recommend a strict protocol after any switch: weekly blood tests for at least four weeks. Some centers require daily checks for the first week. That’s expensive and exhausting. But it’s cheaper than a rejected kidney or liver.
What You Can Do
If you’re on cyclosporine or tacrolimus, here’s what matters:- Stick with one generic brand. Don’t let your pharmacy switch you unless you’re warned and monitored.
- Know your levels. Keep a log of your last three blood test results. If your level drops or spikes by more than 20%, call your transplant team immediately.
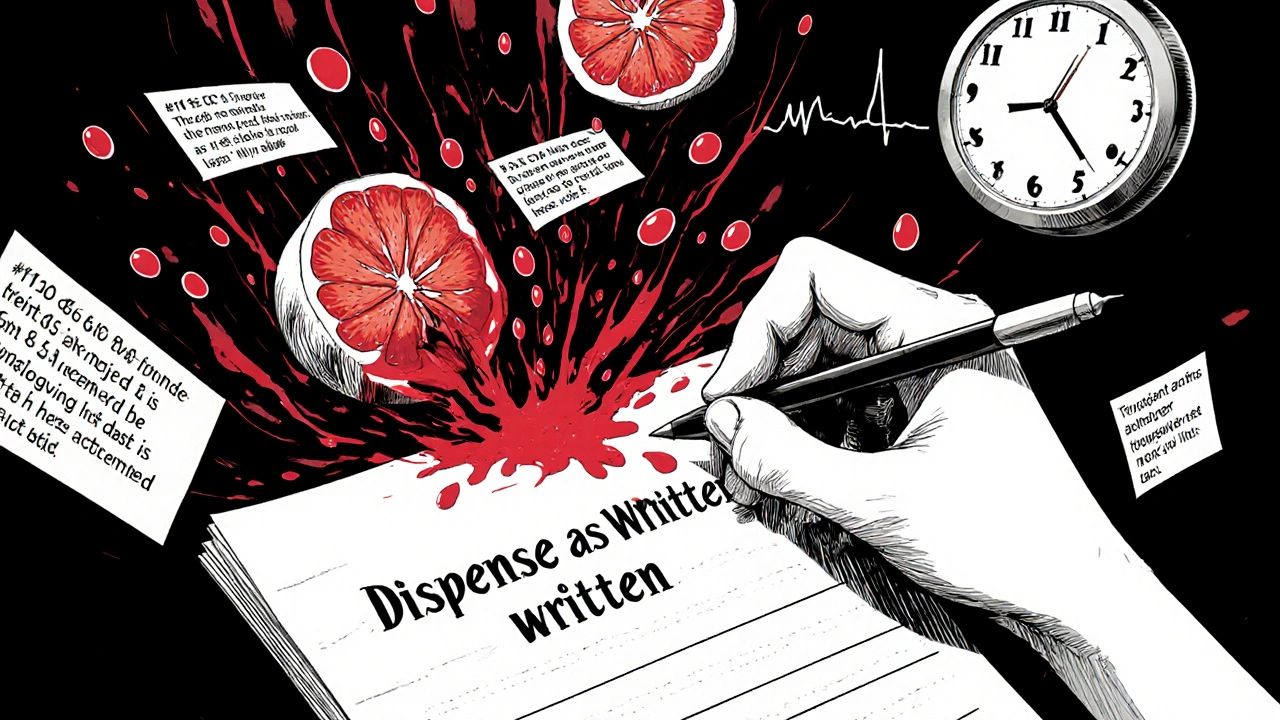
- Avoid grapefruit. It interferes with how these drugs are broken down. Even one grapefruit can cause a dangerous spike.
- Take your dose at the same time every day. A 2-hour window is okay. A 6-hour swing? That’s asking for trouble.
- Ask for a written prescription. If your insurance forces a switch, ask your doctor to write “Dispense as written” or “Do not substitute.” It’s legal in most states.
Some patients worry about cost. But if your insurance pushes you to a cheaper generic, ask if you can stay on the same one long-term. Many centers now sign contracts with pharmacies to supply only one generic brand to avoid switching chaos.
The Future: Better Options
In December 2023, the FDA approved a new extended-release version of tacrolimus called LCP-tacrolimus. It releases the drug slowly, reducing the peaks and valleys in blood levels. That means fewer fluctuations - and less risk when switching generics.Another breakthrough? Genetic testing. Some patients have a gene variant (CYP3A5) that makes them break down tacrolimus faster. If you’re one of them, you need a higher dose. Testing for this before starting the drug can cut the time to reach stable levels by over 60%. More transplant centers are starting to offer it.
The bottom line? Generics are essential for affordability. But with drugs like cyclosporine and tacrolimus, stability is more valuable than savings. A $500 monthly savings means nothing if you lose your transplant.
What’s Next for Patients
If you’re considering a switch, talk to your transplant team - not your pharmacist or insurance rep. Ask: “Which generic brand are you prescribing? Will you monitor my levels closely after the switch?” If they say, “It’s just a generic, it’s fine,” find a second opinion. This isn’t a routine medication. It’s life-sustaining.Organizations like the National Transplant Insurance Assistance Fund help patients fight insurance-mandated switches. You’re not alone. And your voice matters. If you’ve had a bad experience with a generic switch, share it. Patient stories are what change policies.
Can I safely switch between different generic versions of tacrolimus?
No - not without close monitoring. Even though all generics meet FDA standards, differences in how they’re made can cause your blood levels to swing. One patient switched from one generic to another and had a rejection episode because their tacrolimus level dropped 40%. Always stay on the same generic brand unless your transplant team approves a switch and agrees to weekly blood tests for at least a month.
Why is cyclosporine harder to generic than tacrolimus?
Cyclosporine is a large, oily molecule that doesn’t dissolve well in water. Different manufacturers use different oils and additives to help it absorb, and even small changes affect how much gets into your blood. Tacrolimus is smaller and more soluble, so generics are more consistent - but still not perfect. Both need careful monitoring, but cyclosporine has more variability between brands.
Is brand-name Prograf or Neoral still worth the cost?
If you’re stable on brand-name and can afford it, yes. But if you’re on a generic and doing well - no need to switch back. The key isn’t brand, it’s consistency. Many patients are stable on generics for years. The problem isn’t generics themselves - it’s switching between them. If your insurance forces a switch, demand monitoring.
What should I do if my levels drop after switching to a generic?
Call your transplant team immediately. A drop in tacrolimus below 5 ng/mL or cyclosporine below 100 ng/mL in the first six months post-transplant raises rejection risk. You may need a dose increase or a switch back to your previous brand. Don’t wait for symptoms - rejection can happen without pain or fever.
Can I use over-the-counter supplements with these drugs?
Avoid most. St. John’s wort, echinacea, and grapefruit juice can dangerously interfere with how your body processes cyclosporine and tacrolimus. Even common vitamins like vitamin E or fish oil can affect absorption. Always check with your transplant pharmacist before taking anything new - even if it’s labeled “natural.”

Deepa Lakshminarasimhan
November 14, 2025 AT 10:21so i switched to generic tacrolimus last year because my insurance said no choice. first month, i was fine. second month, my creatinine shot up. i thought it was dehydration. third month, i got called in for a biopsy. they said rejection. turns out the generic they gave me? different manufacturer than before. no one warned me. now i pay out of pocket just to stay on the same one. they say 'it's the same drug' like that means anything when your body is a warzone.
Erica Cruz
November 15, 2025 AT 06:50Oh please. This is just fearmongering dressed up as medical advice. The FDA approves these generics. If they weren’t safe, they wouldn’t be on the market. People who panic over 20% absorption variance are the same ones who think their coffee causes cancer. You’re not special. Your body isn’t a magic potion. Just take the pill and stop crying.
Johnson Abraham
November 15, 2025 AT 15:17lol @ericacruz u sound like a pharma rep. i switched generics 3x in 18 mos. each time my levels went nuts. one time i was dizzy for 3 days. doc said 'it's just a generic'... yeah right. now i only take the one brand my pharmacist swears by. and no, i don't trust 'FDA approved' anymore. #pharmabullshit
Shante Ajadeen
November 16, 2025 AT 04:15Thank you for sharing this. I’ve been on generic tacrolimus for 2 years now and I’ve been lucky-no issues. But I never let them switch me to a different brand. I even asked my pharmacy to note it in my file: 'Do Not Substitute.' It’s not about being paranoid. It’s about being smart. If you’re stable, don’t mess with it. Your transplant is worth the extra $50 a month.
dace yates
November 17, 2025 AT 11:53Wait-so if bioequivalence is 80-125%, that means one generic could be half as strong as another? That doesn’t seem like 'equivalent' to me. Is there any data on how many patients actually get rejected because of this? Or is it all anecdotal?
Danae Miley
November 19, 2025 AT 10:28It’s not anecdotal. A 2022 multicenter study published in *Transplantation* tracked 412 patients who switched generics. 18% had clinically significant rejection episodes within 6 weeks. Another 23% required urgent dose adjustments. The FDA’s bioequivalence standard was designed for antibiotics, not NTI immunosuppressants. This is a regulatory failure disguised as cost-saving.
Charles Lewis
November 20, 2025 AT 04:50Let me offer a broader perspective. The issue isn’t merely about generics-it’s about the fragmentation of pharmaceutical supply chains, the lack of pharmacovigilance in post-market drug transitions, and the systemic pressure on transplant centers to reduce costs at the expense of patient stability. We are treating life-sustaining medication like commodity goods, when in reality, these drugs are not interchangeable in the same way as ibuprofen or omeprazole. The clinical protocols must evolve to reflect the biological reality of individual variability, not the economic convenience of insurance networks. This isn’t a drug problem-it’s a healthcare design failure.
Renee Ruth
November 21, 2025 AT 23:14I had a kidney transplant in 2019. Switched to generic tacrolimus in 2021. Three weeks later, I was in the ER with fever, chills, and my creatinine at 5.2. They said it was 'just a virus.' I begged them to check levels. They did. Tacrolimus was at 2.1 ng/mL. I had a biopsy. Rejection. ICU. 7 days. $87,000 bill. Insurance won’t cover brand now. I’m stuck. My doctor says 'it’s fine' but I know better. I sleep with my blood test results under my pillow. I’m not crazy. I’m surviving.
Samantha Wade
November 22, 2025 AT 07:34Every transplant patient deserves stability-not a game of pharmaceutical roulette. The fact that we’re even having this conversation is a tragedy. If your insurance forces a switch, demand a written exception. File a grievance. Contact your state’s insurance commissioner. Join patient advocacy groups. Your life is not a spreadsheet. And if your doctor says 'it’s just a generic,' find a new doctor. There are centers that prioritize patient safety over corporate contracts. You are not alone. Fight.
Elizabeth Buján
November 23, 2025 AT 16:29it’s wild how something so small-like a different filler in a pill-can change your whole life. i used to think meds were meds. now i know: your body remembers every change. i’ve been on the same generic for 4 years. no drama. no spikes. no scares. but i never let them switch me. i write it on my calendar. i call my pharmacy every month. i’m not being obsessive. i’m being alive. if you’re reading this and you’re stable? hold on to that. don’t let anyone take it from you. your transplant is your miracle. protect it.
Andrew Forthmuller
November 24, 2025 AT 02:50grapefruit bad. take at same time. log levels. dont switch generics. got it. simple.
vanessa k
November 24, 2025 AT 19:38My brother’s on tacrolimus. He switched generics last year because his insurance changed. He didn’t tell anyone. Thought it was 'just a pill.' Two months later, he had a seizure. Turns out his levels were at 0.8 ng/mL. He’s okay now, but he’s terrified. He won’t even let his pharmacist refill without calling his doctor first. I just want people to know: this isn’t theoretical. It’s real. And it happens more than you think.