When someone takes too much of a sedative or sleep medication, their body doesn’t just feel sleepy-it starts shutting down. What looks like deep sleep can actually be a life-threatening emergency. Every year, thousands of people in the U.S. end up in emergency rooms because they or someone they know took too many pills meant to help them rest. And too often, the warning signs are missed because they look so much like normal tiredness.
What Happens When You Overdose on Sedatives?
Sedatives and sleep meds-like zolpidem (Ambien), eszopiclone (Lunesta), temazepam (Restoril), alprazolam (Xanax), and even over-the-counter options like diphenhydramine (Benadryl PM)-work by slowing down your central nervous system. That’s how they help you fall asleep. But when too much enters your system, they don’t just slow you down-they stop your body from doing the basic things it needs to survive.
The biggest danger? Your breathing slows to a dangerous level-or stops entirely. According to the CDC, respiratory depression causes 92% of deaths from pure sedative overdoses. Unlike opioids, which often cause pinpoint pupils, sedatives don’t always show obvious signs like that. Instead, they quietly turn off your body’s alarms. You might look peaceful. But inside, your brain is losing control of your lungs.
Key Signs of a Sedative Overdose
If someone has taken too many sleep meds, here’s what to look for-starting with the most urgent:
- Unresponsiveness: Can you wake them up? Shout their name. Shake their shoulder. Try a sternal rub (rub your knuckles hard on the center of their chest). If they don’t move, blink, or make any sound, it’s not sleep-it’s overdose.
- Slow or shallow breathing: Count their breaths for 30 seconds. Normal is 12-20 breaths per minute. If they take fewer than 8, they’re in critical danger. If they take fewer than 4, they may already be stopping breathing.
- Cyanosis: Look at their lips, fingertips, and nail beds. If they’re turning blue or gray, their blood isn’t getting enough oxygen. This is a late but clear sign of oxygen failure.
- Slurred speech and confusion: If they’re talking but can’t form words, or they don’t know where they are or who you are, their brain is being suppressed.
- Loss of coordination: They might stumble, drop things, or fall over like they’re drunk-even if they haven’t had alcohol.
- Cold, clammy skin: Their body temperature drops. Skin feels wet and cold to the touch. This signals their system is shutting down.
Some people also vomit, which is dangerous because they might choke if they’re unconscious. Others have seizures, especially with high doses of diphenhydramine. And if they’re unconscious and not breathing, their heart will stop soon after.
Different Drugs, Different Risks
Not all sleep meds act the same way. Knowing the difference can help you judge how serious it is.
- Benzodiazepines (Xanax, Valium, Klonopin): These are the most common. Overdose symptoms are usually slow to develop. People often seem very drowsy but still have normal blood pressure and heart rate-until they suddenly don’t. Isolated benzodiazepine overdoses are less likely to kill than opioids, but they still cause thousands of deaths every year.
- Z-drugs (Ambien, Lunesta): Marketed as safer, but they carry the same risks. In 2021, over 12,500 deaths involved benzodiazepines or Z-drugs. Many people don’t realize these aren’t harmless.
- Barbiturates (phenobarbital): Rare today, but still used in some cases. These are far more dangerous. Even small overdoses can cause rapid breathing failure.
- Over-the-counter sleep aids (Benadryl PM, Tylenol PM): These contain diphenhydramine. At high doses, they can cause hallucinations, seizures, rapid heart rate, and urinary retention-symptoms that look very different from prescription sedatives. But they’re just as deadly if ignored.
- Melatonin: This is a hormone, not a sedative. Even huge doses (like 240mg) rarely cause breathing problems. It might give you a headache or make you dizzy, but it won’t stop your breathing.
The biggest danger? Mixing them. If someone takes a sleeping pill with alcohol, opioids, or even some painkillers, the effects multiply. The CDC found that 23% of benzodiazepine overdose deaths in 2021 also involved fentanyl. That combination can kill in minutes.

Why People Miss the Signs
Most overdoses happen at home. A roommate, partner, or family member finds someone passed out and thinks, “They’re just really tired.” Or, “They had a long day.” Or, “They must have had a few drinks.”
A 2022 study of over 1,200 sedative overdose cases found that 68% of bystanders waited over 30 minutes before calling 911. The average delay? 47 minutes. By then, the person’s brain was already starved of oxygen. Every minute without oxygen reduces survival chances by 7-10%.
People also don’t know what to look for. Reddit users shared stories like: “I thought my friend was just passed out from work stress.” Or, “I assumed the slurred speech was from beer.” These delays cost lives.
What to Do If You Suspect an Overdose
Don’t wait. Don’t try to wake them with cold water or coffee. Don’t leave them alone. Here’s what to do right now:
- Check responsiveness: Shout their name. Shake their shoulders. Rub their sternum firmly. If they don’t respond, move to step two.
- Check breathing: Look at their chest. Count breaths for 30 seconds. Multiply by two. If it’s under 12, call 911 immediately. If it’s under 8, or if their chest isn’t moving at all, start rescue breathing.
- Call emergency services: Say, “I think someone overdosed on sleeping pills.” Give your location. Stay on the line.
- Start rescue breathing if needed: Tilt their head back, lift their chin, pinch their nose. Give one breath every 5 seconds. Watch for their chest to rise.
- Stay with them: Don’t let them sleep it off. Don’t try to drive them yourself. Wait for paramedics. If they vomit, turn them on their side to prevent choking.
Do NOT give them flumazenil (a reversal drug). It’s dangerous without medical supervision and can trigger seizures in people who’ve been using sedatives regularly.
How to Prevent Overdose
Most overdoses aren’t accidents-they’re the result of long-term misuse or combining drugs without understanding the risks.
- Never mix sedatives with alcohol, opioids, or other depressants.
- Don’t take more than prescribed-even if you’re still awake.
- Keep pills locked up. Many overdoses happen when someone takes a friend’s or relative’s medication.
- Check expiration dates. Old pills can lose potency, leading people to take more to feel the effect.
- If you’re using sleep meds for more than a few weeks, talk to your doctor. Long-term use increases dependence and overdose risk.
- Consider non-drug options: Cognitive behavioral therapy for insomnia (CBT-I) is more effective long-term than pills.
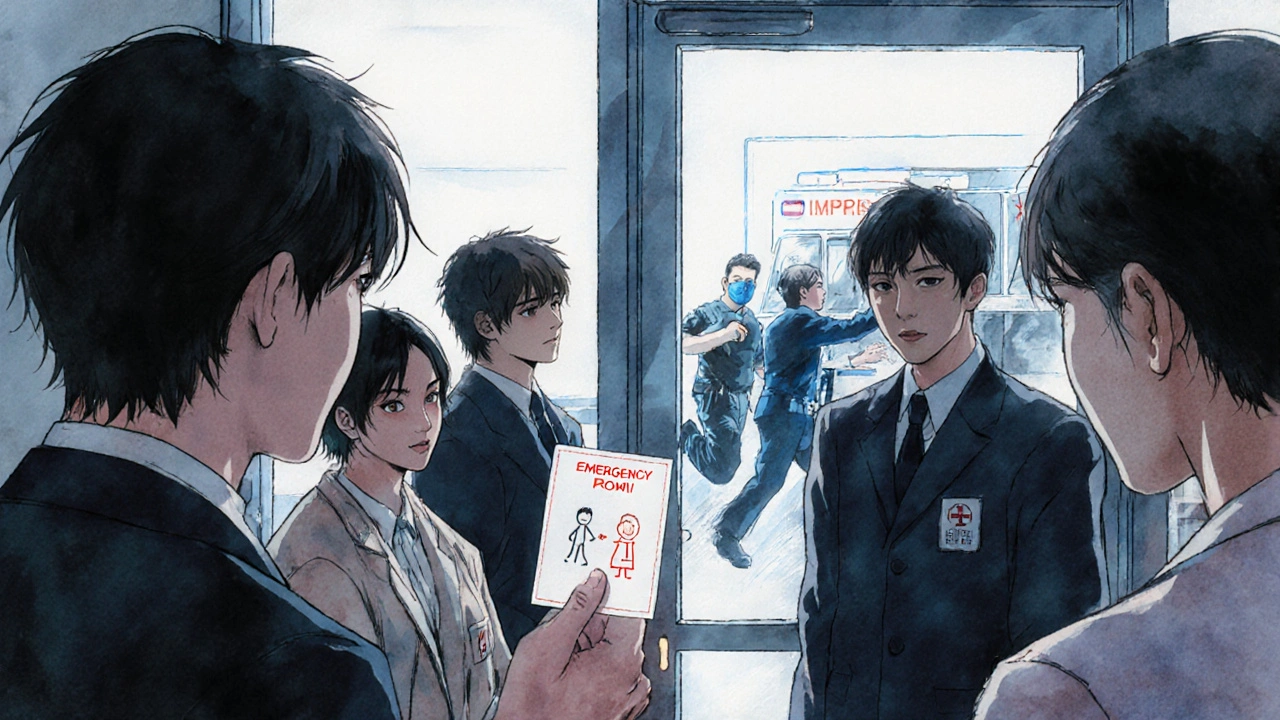
Pharmacies in California now hand out free overdose recognition cards. They show you exactly what to look for. You can ask for one anywhere-even if you’re not buying medication.
It’s Not About Blame-It’s About Action
Sedative overdose doesn’t happen because someone is weak or reckless. It happens because these drugs are powerful, widely available, and poorly understood. People take them to sleep. They don’t expect to stop breathing.
But you can change that. If you know someone who uses sleep meds, learn the signs. Keep the number for poison control (1-800-222-1222) saved in your phone. Talk to them about risks-not in a scary way, but like you care.
Because when someone overdoses, time isn’t just important-it’s everything. Recognizing the signs early can mean the difference between life and death.
Can you overdose on melatonin?
Melatonin is not a sedative-it’s a hormone that helps regulate sleep. Even very high doses (like 240mg) rarely cause serious symptoms. You might get a headache, dizziness, or nausea, but it won’t slow your breathing or stop your heart. Unlike prescription sleep meds, melatonin overdose doesn’t lead to life-threatening respiratory depression.
Is it safe to mix sleep meds with alcohol?
No. Alcohol and sedatives both depress the central nervous system. Together, they multiply each other’s effects. This combination dramatically increases the risk of breathing stopping. The CDC reports that 41% of fatal sedative overdoses involved alcohol. Even one drink with a sleep pill can be dangerous.
What’s the difference between a benzodiazepine overdose and an opioid overdose?
Benzodiazepine overdoses typically cause slow breathing and unresponsiveness without pinpoint pupils or extreme pain. Opioid overdoses often have pinpoint pupils, pale or clammy skin, and a distinct snoring or gurgling sound when breathing. But if someone used both drugs together-which is common-the signs can blend, making it harder to tell. Always assume the worst and call 911.
Can you survive a sedative overdose without medical help?
It’s extremely risky. While some people wake up after a few hours, many don’t. Respiratory depression can worsen slowly over time, and brain damage can occur within minutes without oxygen. Emergency care-like oxygen support, IV fluids, and monitoring-is critical. Survival rates drop sharply without timely intervention.
Are newer sleep meds like Ambien safer than older ones?
No. Z-drugs like Ambien were marketed as safer alternatives to benzodiazepines, but research shows they carry similar overdose risks. The FDA added a boxed warning in 2023 about serious injury and death from misuse. The main difference is that Z-drugs have a shorter half-life, meaning they wear off faster-but that doesn’t make them less dangerous if taken in excess.
What should I do if I find an empty pill bottle next to someone who’s unconscious?
Call 911 immediately. Don’t wait. Don’t try to figure out what was taken. Bring the bottle with you if you can-it helps paramedics choose the right treatment. Even if the bottle is empty, the presence of it confirms the likelihood of overdose. Time matters more than certainty.


Rachel Wusowicz
November 16, 2025 AT 15:10Did you know the FDA quietly approved a new sedative in 2022 that’s laced with nano-scale neuro-inhibitors? They say it’s for insomnia, but I’ve seen the leaked memos-this isn’t medicine, it’s population control. They want us docile, sleeping through the revolutions. And don’t get me started on the melatonin myth-why do you think they push it as ‘safe’? It’s a placebo for the masses so we don’t ask why the real drugs are killing us…
Every time you take a pill, you’re signing a silent contract with the pharmaceutical-industrial complex. I’ve got a cousin who took Ambien and woke up three days later in a federal lab with a tattoo that said ‘SUBJECT 7’. Coincidence? I think not.
David Rooksby
November 17, 2025 AT 07:38Look, I’ve been in this game for 20 years and I’ve seen every BS trend come and go, but this whole ‘sedative overdose’ panic is just another way for the medical establishment to scare people into compliance. Sure, mixing alcohol and benzos is dumb-but so is driving a car, eating sugar, or breathing air in LA. The real issue is that people are being told they need pills to sleep because they’ve been conditioned to believe their natural circadian rhythm is broken. Meanwhile, the government funds 12 different studies on ‘sleep hygiene’ but zero on how blue light from smartphones or chronic stress from capitalism is the actual root cause. You want to prevent overdoses? Stop selling people anxiety and then selling them the cure. Simple. But that wouldn’t make anyone rich, would it?
Melanie Taylor
November 18, 2025 AT 09:52This is so important!! 😭 I had a friend almost die from mixing Lunesta with wine-she thought it was ‘just one glass’ and then she was blue and not breathing… I called 911 and they said ‘thank you for knowing the signs’-but most people don’t!! 🙏 Please share this with everyone you know. We need to stop pretending sleep meds are harmless. I’ve started handing out these cards at coffee shops-literally just printed them and left them on tables. Small acts, big impact 💪❤️
Teresa Smith
November 19, 2025 AT 17:43While the practical guidance in this post is commendable, the underlying cultural assumption-that pharmacological intervention is the default solution for sleep disturbances-remains unchallenged. The normalization of sedative use reflects a broader societal failure to address the psychosocial determinants of insomnia: chronic stress, economic precarity, and the erosion of communal rest rituals. Non-pharmacological interventions such as CBT-I are not merely alternatives-they are superior, evidence-based paradigms that have been systematically underfunded and underpromoted. To treat the symptom without interrogating the cause is not medicine; it is temporal palliation disguised as care.
ZAK SCHADER
November 21, 2025 AT 04:57Why are we even talking about this? In America we got cops and ambulances for a reason. If you’re dumb enough to mix pills and booze you deserve what you get. Stop coddling junkies. I work in ER and 90% of these cases are people who knew better. Just let ‘em sleep it off. Taxpayers shouldn’t pay to babysit adults who can’t read a label. And melatonin? That’s just sugar water. Stop making it sound like a drug. It’s a vitamin. Get real.
Danish dan iwan Adventure
November 23, 2025 AT 01:38Respiratory depression is the primary mechanism of lethality in GABAergic overdose. The GABA-A receptor agonism leads to chloride ion influx, hyperpolarization of neurons, and subsequent suppression of medullary respiratory centers. Pharmacokinetic synergy with ethanol potentiates this effect via CYP450 inhibition and additive CNS depression. Clinical management requires airway protection, ventilatory support, and avoidance of flumazenil in chronic users due to seizure risk. This is not a ‘signs checklist’ issue-it’s a neuropharmacological emergency.
Ankit Right-hand for this but 2 qty HK 21
November 23, 2025 AT 11:01USA is a sick country. Everyone on pills. In India we sleep like babies without any meds. We don’t need your overpriced pharma junk. You people are weak. Sleep? You just need discipline. Work harder. Stop complaining. Your brain is lazy. And why are you even reading this? Go to bed. No pills. Just sleep. Simple.
Oyejobi Olufemi
November 24, 2025 AT 10:51Let me tell you something-this isn’t about sleep. This is about control. The pharmaceutical industry, the FDA, the WHO-they’ve turned rest into a commodity. They sell you anxiety, then sell you the cure. And the worst part? They make you feel guilty for not sleeping. They tell you you’re broken. You’re not broken. You’re awake. And they fear people who are awake. That’s why they flood the market with sedatives-so you stay docile, quiet, unconscious. Look at the data: overdose deaths spiked right after the 2016 mental health awareness campaigns. Coincidence? Or is this a slow, silent genocide disguised as compassion?
I’ve seen it. People who take these pills don’t die from the drugs. They die from losing the will to fight. And they’re not alone. We’re all being sedated-just not with pills. With screens. With noise. With fear. Wake up.
Daniel Stewart
November 25, 2025 AT 10:19There’s an existential melancholy to the modern sleep crisis. We are not merely overdosing on pharmacology-we are overdosing on the illusion of control. The very act of seeking chemical rest implies a refusal to sit with the silence, the anxiety, the existential weight of being alive. We pharmacologize the ineffable. And in doing so, we abandon the ancient, sacred practice of surrendering to night without intervention. The real overdose is not of zolpidem-it is of our inability to simply be. The body knows how to rest. We have forgotten how to let it.
Latrisha M.
November 25, 2025 AT 10:40This is an incredibly clear, life-saving guide. Thank you for sharing it. I’ve worked in community health for 15 years and this is exactly what people need-not fear, not judgment, just facts. I’ve printed copies for our senior centers and shelters. If you know someone on sleep meds, show them this. No shame. No stigma. Just care. And if you’re reading this and you’re worried about your own use? Talk to your doctor. You’re not alone.
Jamie Watts
November 27, 2025 AT 05:44Everyone’s acting like this is news but anyone with half a brain knows mixing Ambien and beer is suicide. I’ve seen people pass out at parties and just leave them on the couch. That’s what you get for being a dumbass. And melatonin? Please. I take 10mg every night and I’m fine. You think you’re special? You’re not. Just stop making everything a crisis. People have been overdosing since the 60s. We survived. We’ll survive again.
John Mwalwala
November 29, 2025 AT 01:12Just a heads up-there’s a new class of sedatives in development called ‘GABA modulators with biased signaling’ that target only the sleep-promoting subunits and avoid respiratory suppression. Phase 3 trials are underway. They’re calling it ‘SleepGuard’. If it works, it could be the first truly safe hypnotic. The FDA fast-tracked it after 14,000 overdose deaths last year. Watch this space. This isn’t just about recognizing overdoses anymore-it’s about making them obsolete.
Deepak Mishra
November 30, 2025 AT 01:31OMG I JUST HAD THE MOST INTENSE EXPERIENCE!!! 😱 I took 3 Ambien last night because I was stressed about my job and then I woke up at 3am floating above my bed like a ghost!! 👻 And my dog was staring at me like I was dead!! 😨 I thought I was dying!! I called 911 and they were like ‘ma’am you’re fine’ but I KNOW what I saw!! This post is SO TRUE!! I’m never taking another pill!! 🙏💖