Getting the right dose of medicine for your child isn’t just about following the label-it’s about avoiding a mistake that could land them in the hospital. Every year, thousands of kids end up in emergency rooms because someone gave them too much-or too little-medication. And the most common cause? Using a kitchen spoon or a dosing cup that doesn’t measure accurately. The truth is, if you’re not using the right tool, you’re guessing-and guessing with your child’s health isn’t an option.
Why Milliliters (mL) Are the Only Measurement That Matters
Stop using teaspoons and tablespoons. Seriously. Even if the bottle says "1 tsp," that’s not safe. A standard kitchen teaspoon can hold anywhere from 3.9 to 7.3 milliliters, while the actual medical teaspoon is exactly 5 mL. That difference might seem small, but for a 12-month-old, it can mean the difference between healing and harm.
The CDC’s PROTECT initiative made it clear: all pediatric liquid medications should be dosed only in milliliters (mL). No more "teaspoon," no more "tablespoon." Why? Because confusion between milligrams (mg) and milliliters (mL) causes nearly 36% of all pediatric dosing errors, according to the Institute for Safe Medication Practices. A parent might think "5 mg" is the same as "5 mL," but they’re completely different. One is a weight, the other is a volume. Mixing them up can lead to a tenfold overdose.
Look at your child’s prescription. If it says "2.5 tsp," ask the pharmacist to rewrite it as "12.5 mL." Most pharmacies still print both, but you don’t need both. You only need mL. And if the label doesn’t match what the doctor said, speak up. You have the right to ask for clarity.
The Right Tool for the Job: Oral Syringes Win Every Time
Not all measuring tools are created equal. Here’s what actually works:
- Oral syringes (1-10 mL): 94% accurate. Best for doses under 5 mL. No spills. No guesswork. Just push the plunger slowly.
- Dosing cups (5-30 mL): 76% accurate. Fine for older kids who can drink directly, but error rates jump to 68% for doses under 5 mL.
- Dosing spoons: 82% accurate. Better than kitchen spoons, but still not as precise as a syringe.
- Kitchen spoons: Never use. They vary by up to 200%. One family’s "teaspoon" might be 3 mL, another’s 10 mL.
A 2020 study of 497 parents showed that when measuring 2.5 mL, dosing cups failed nearly 7 out of 10 times. Oral syringes? Only 1 in 8 got it wrong. That’s why the CDC recommends oral syringes as the preferred tool for any dose under 5 mL. If your child’s medicine is 1.5 mL or 3 mL? Use a syringe. Always.
Pro tip: Buy syringes with clear markings and a wide barrel. Some brands, like NurtureShot and Medisana BabyDos, have color-coded tips for different doses and even come with a cap to prevent spills. They’re cheap-usually under $15-and often given out for free at pediatric clinics.
How to Measure Liquid Medicine Accurately
Even the best tool won’t help if you don’t use it right. Here’s how to get it perfect every time:
- Shake the bottle-especially antibiotics or suspensions. If it’s thick and cloudy, the medicine settles. Not shaking means your child gets less than half the dose.
- Draw the liquid slowly into the syringe. Don’t rush. Let it fill naturally.
- Hold the syringe upright at eye level. Look at the plunger, not the side of the barrel.
- Read the meniscus-the curved surface of the liquid. Line up the top of the curve with the correct mL mark. Don’t guess. Don’t eyeball.
- Give it slowly into the side of the mouth (cheek pouch), not the front. Kids spit out medicine if it hits their tongue too hard.
Some parents mark their syringes with a permanent marker-"2.5 mL" next to the line-so they don’t have to read it every time. That’s smart. Especially if your child takes the same medicine daily.

Weight Matters: Calculating the Right Dose
Most children’s medications are dosed by weight: milligrams per kilogram (mg/kg). That means if your child gains weight, their dose changes. You can’t use the same dose forever.
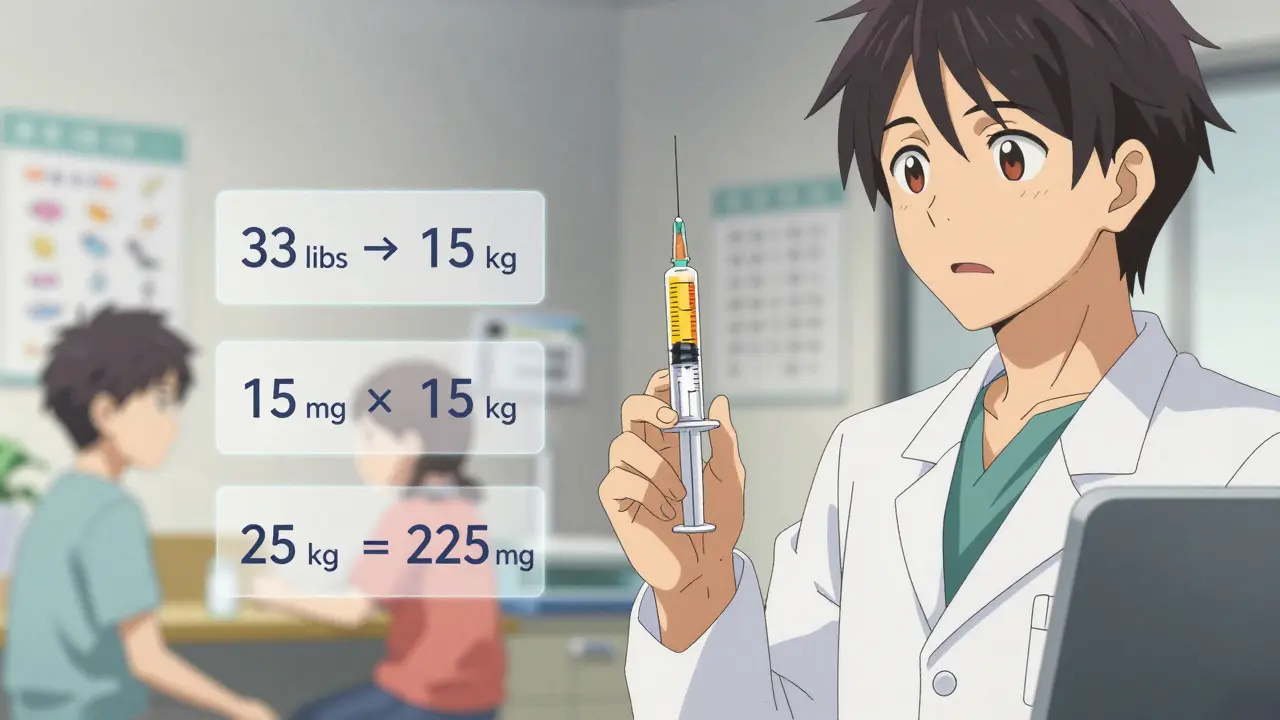
Here’s how to convert pounds to kilograms: Divide weight in pounds by 2.2. Example: A child weighing 33 pounds is 33 ÷ 2.2 = 15 kg.
Now, if the prescription says "15 mg/kg twice daily," and your child weighs 15 kg, that’s 15 × 15 = 225 mg per dose. If the medicine is 150 mg per 5 mL, then each dose is 7.5 mL.
Don’t do this math in your head. Write it down. Use a calculator. Ask your pharmacist to double-check it. Many pharmacies now have apps that auto-calculate doses based on weight. Ask if yours does.
Common Mistakes (And How to Avoid Them)
Parents make the same errors over and over. Here’s what to watch out for:
- Using the wrong syringe-like one meant for insulin (1 mL) instead of a pediatric syringe (5 mL). Insulin syringes are too small and easy to misread.
- Not checking the concentration-amoxicillin can be 125 mg/5 mL or 250 mg/5 mL. Same bottle, different strength. Always confirm.
- Sharing syringes-don’t use the same syringe for different medicines. Clean it after each use, but don’t cross-contaminate.
- Forgetting to shake-as many as 50% of parents skip this step with suspensions. Result? Under-dosing.
- Using kitchen utensils-yes, even if "it’s just a little." That "little" could be 2 mL too much.
One mother in Melbourne told us she gave her 2-year-old the wrong dose because she used a coffee spoon. Her child got sick. She learned the hard way. Now, she keeps a labeled syringe in her diaper bag. Simple. Safe.
What to Do If You’re Unsure
If you’re confused, stop. Don’t guess.
- Call your pharmacist. They’re paid to answer these questions.
- Ask your pediatrician to write the dose in mL only.
- Request a dosing chart from your clinic. Many hospitals give out printed guides with weight-based dosing for common meds like acetaminophen and ibuprofen.
- Use a trusted app like MedSafety, which uses augmented reality to show you exactly where to fill the syringe.
Don’t feel embarrassed. You’re not alone. Studies show 7 in 10 parents make at least one dosing mistake in the first year. The goal isn’t perfection-it’s awareness. And awareness saves lives.
Special Cases: Narrow Therapeutic Index Medications
Some medicines are powerful and dangerous if dosed wrong. Think digoxin, warfarin, or certain seizure meds. Even a 1 mL error can cause serious harm.
For these, only use an oral syringe. Never a cup. Never a spoon. Always double-check with your pharmacist. Keep a written log of each dose. If your child takes one of these, ask your doctor for a written dosing schedule. Tape it to the fridge. Review it every time you give medicine.
What’s Changing in 2026
The FDA is pushing for a new rule: all pediatric liquid medications must come with a standardized mL-only oral syringe. That’s happening in 2024-2025. By 2026, nearly every prescription for a child’s liquid medicine will include the right tool in the box.
Pharmacies are also starting to offer free syringes at pickup. If yours doesn’t, ask. Some clinics now give them out during well-child visits. You don’t have to buy them-just ask.
Color-coding is catching on too. Red syringes for antibiotics. Blue for pain relievers. It’s not magic-but it helps. Especially when multiple caregivers are involved.
Final Rule: Always Use the Tool That Came With the Medicine
That little plastic syringe? Keep it. Don’t toss it after one use. Store it in a ziplock bag with the bottle. Label it with your child’s name. That’s your go-to tool. Never substitute.
And if you’re ever in doubt? Call your doctor or pharmacist before giving the dose. Better safe than sorry. One phone call could prevent a hospital visit.
Can I use a kitchen teaspoon if I don’t have a syringe?
No. Kitchen teaspoons vary in size by up to 200%. A standard teaspoon is 5 mL, but yours might hold 3 mL or 8 mL. That’s too risky for a child. Always use the tool that came with the medicine-or buy an oral syringe. They cost less than $5 and are far safer.
What if my child spits out the medicine?
Try giving it slowly into the cheek pouch, not the front of the mouth. You can also mix the dose with a small spoonful of applesauce or yogurt-but only if the medicine allows it. Check the label or ask your pharmacist. Never mix with juice or milk unless told it’s safe. And if your child spits out more than half, call your doctor. They’ll tell you whether to give another dose.
Do I need to clean the syringe after each use?
Yes. Rinse it with warm water after each use. Don’t boil it or put it in the dishwasher unless the manufacturer says it’s safe. Let it air-dry. Store it in a clean bag. Never reuse a syringe for a different medicine without washing it thoroughly.
How do I know if my child’s dose is too high or too low?
Signs of under-dosing: fever doesn’t go down, infection gets worse, symptoms last longer than expected. Signs of overdosing: vomiting, drowsiness, confusion, rash, or trouble breathing. If you suspect an overdose, call Poison Control immediately (1-800-222-1222 in the U.S. or your local emergency number). For under-dosing, call your pediatrician. Don’t wait.
Are there apps that help with dosing?
Yes. Apps like MedSafety and Pediatric Dose Calculator use augmented reality to show you exactly how much to draw up. Some even scan the medicine bottle and auto-calculate the dose based on your child’s weight. They’re not perfect, but they reduce errors by over 50%. Always double-check with your pharmacist, but these tools are helpful for busy parents.

Jack Havard
February 13, 2026 AT 18:13Let’s be real - if you’re relying on a syringe because you can’t trust yourself to eyeball a teaspoon, maybe you shouldn’t be administering medicine at all. I’ve given my kid meds for years with a kitchen spoon and zero issues. The stats are inflated. Hospitals love scare tactics to sell you gear. You don’t need a $15 syringe. You need common sense.
Also, who decided milliliters were the gold standard? Why not drops? Or grams? Why does the CDC get to dictate how I parent? I’ll use what works for my family, thanks.
Luke Trouten
February 13, 2026 AT 18:43There’s a deeper philosophical tension here between institutional authority and personal autonomy in caregiving. The medical establishment promotes standardization as a safeguard, yet in doing so, it risks eroding parental intuition - a deeply human, adaptive mechanism honed over millennia.
While precision is objectively valuable, especially with narrow therapeutic index drugs, blanket mandates may inadvertently foster dependency on tools rather than understanding. The goal should be empowerment, not compliance. A parent who grasps why 5 mL ≠ 1 tsp is more resilient than one who simply owns a syringe.
Gabriella Adams
February 14, 2026 AT 04:48I work in pediatric nursing, and I can tell you - this post is 100% accurate. I’ve seen too many kids come in with toxicity from "a little extra" or sepsis from under-dosing because someone used a coffee spoon.
It’s not about fear-mongering. It’s about physics. A kitchen spoon isn’t calibrated. It’s not a medical device. And your child’s body doesn’t care if you "mean well."
Buy a $3 syringe. Keep it with the bottle. Label it. Use it. It’s not complicated. And if you’re worried about cleaning it - rinse it with warm water. That’s it. No magic required. Just consistency.
Brad Ralph
February 15, 2026 AT 08:52So the CDC wants us to use syringes... and also gave us a 20-year pandemic response that included mask mandates and vaccine passports. Coincidence? 🤔
Jk. Sorta. But seriously - if you're using a syringe, you're already ahead of 80% of parents. Just don’t forget to wash it. I’ve seen people use the same syringe for Tylenol, antibiotics, and melatonin. That’s not a medical tool. That’s a biohazard.
Suzette Smith
February 15, 2026 AT 21:42I get why you’re pushing syringes, but what about parents who can’t afford them? Or who don’t have access to pharmacies? I live in a rural area - the nearest pharmacy is 45 minutes away. I’ve used a measuring spoon for three kids. None of them have been hospitalized. Maybe the problem isn’t the spoon - it’s the system that makes tools inaccessible.
Autumn Frankart
February 16, 2026 AT 18:09Let me guess - this was written by Big Pharma. Who benefits from parents buying syringes? Who profits when you're told your kitchen tools are "dangerous"? The same companies that sold you formula with lead, vaccines with adjuvants, and baby food with arsenic.
They want you dependent. They want you scared. They want you to trust them over your own instincts.
And now they’re telling you to stop using spoons? That’s not safety. That’s control. Wake up.
My child survived. Your child will too. Trust your gut. Not the FDA.
Skilken Awe
February 17, 2026 AT 08:24Wow. A 76% accuracy rate for dosing cups? That’s statistically irrelevant. You’re treating this like a clinical trial, not parenting.
Also, "oral syringes are 94% accurate" - based on what? A study of 497 parents who were handed syringes and told to use them? Of course they’re better - because they were given instructions.
Real-world data? My cousin gave her kid 3 mL with a spoon. Kid’s fine. Kid’s now a neurosurgeon. Coincidence? I think not.
Stop weaponizing precision. You’re making parents feel guilty for being human.
Ernie Simsek
February 19, 2026 AT 01:17Bro. I used a turkey baster once to give my kid amoxicillin. He didn’t die. He’s now in college. 🤷♂️
Look - I get it. Syringes are ideal. But you’re acting like this is a life-or-death nuclear code launch. It’s not. Kids are way more resilient than we think.
Also - why is no one talking about the fact that 80% of these meds are sugar water with a hint of active ingredient? We’re treating kids like lab rats. Chill.
Reggie McIntyre
February 20, 2026 AT 23:50One of the most beautiful things about parenting is how we adapt - sometimes with syringes, sometimes with droppers, sometimes with a teaspoon and a prayer.
But here’s the thing: if you’ve ever stared at a 1.5 mL dose in a syringe, felt your hands shake, and thought "I hope I got this right," you’re not alone.
That’s why tools matter. Not because we’re incompetent - but because love makes us careful. And care deserves precision.
Keep the syringe. Keep the calm. Keep trusting yourself - but give yourself the best shot.
Carla McKinney
February 22, 2026 AT 05:06Let’s not romanticize "common sense." Common sense is why people still give aspirin to kids. Common sense is why we used lead paint. Common sense is why we thought thalidomide was safe.
Medicine isn’t decided by anecdotes. It’s decided by data. The data says: syringes reduce errors by 80%. Kitchen spoons cause 36% of dosing errors.
If you’re not using a syringe, you’re not being responsible. You’re being reckless. And yes - I’m saying that to your face.
Ojus Save
February 22, 2026 AT 13:55i use a spoon n my kid is fine. maybe u shud try it. also why u need a syringe? its too much work. just give it in mouth. easy. no need to overthink. my mom did it n we all grew up. 🤷♂️
Gloria Ricky
February 22, 2026 AT 20:53My son had a fever last week. I used the syringe that came with the medicine - and I swear, it felt like a tiny act of love.
Shaking the bottle. Holding it at eye level. Slow push. He didn’t spit it out. He smiled. I cried a little.
It’s not about the tool. It’s about showing up. And yeah - the tool helps you show up better.
PS: I got mine free from the clinic. Just ask.
Stacie Willhite
February 23, 2026 AT 19:49I just wanted to say thank you for writing this. I gave my daughter the wrong dose last month because I used a tablespoon thinking "it’s just a little more." She was fine, but I haven’t stopped shaking since.
I bought a syringe yesterday. I labeled it. I keep it in her diaper bag. I’m not perfect - but I’m trying.
If you’re reading this and you’re scared - you’re not alone. We’re all just trying to keep our kids safe.
Jason Pascoe
February 23, 2026 AT 22:44As someone who’s given meds to kids in three countries - Australia, Canada, and the US - I can say this: the syringe advice is universal.
It’s not about fear. It’s about consistency. A teaspoon in Melbourne isn’t the same as one in Atlanta. But 5 mL? That’s the same everywhere.
And yes - I’ve seen parents use a syringe meant for insulin. That’s worse than using a spoon.
Ask your pharmacist for the right one. They’ll give it to you. No shame. Just safety.