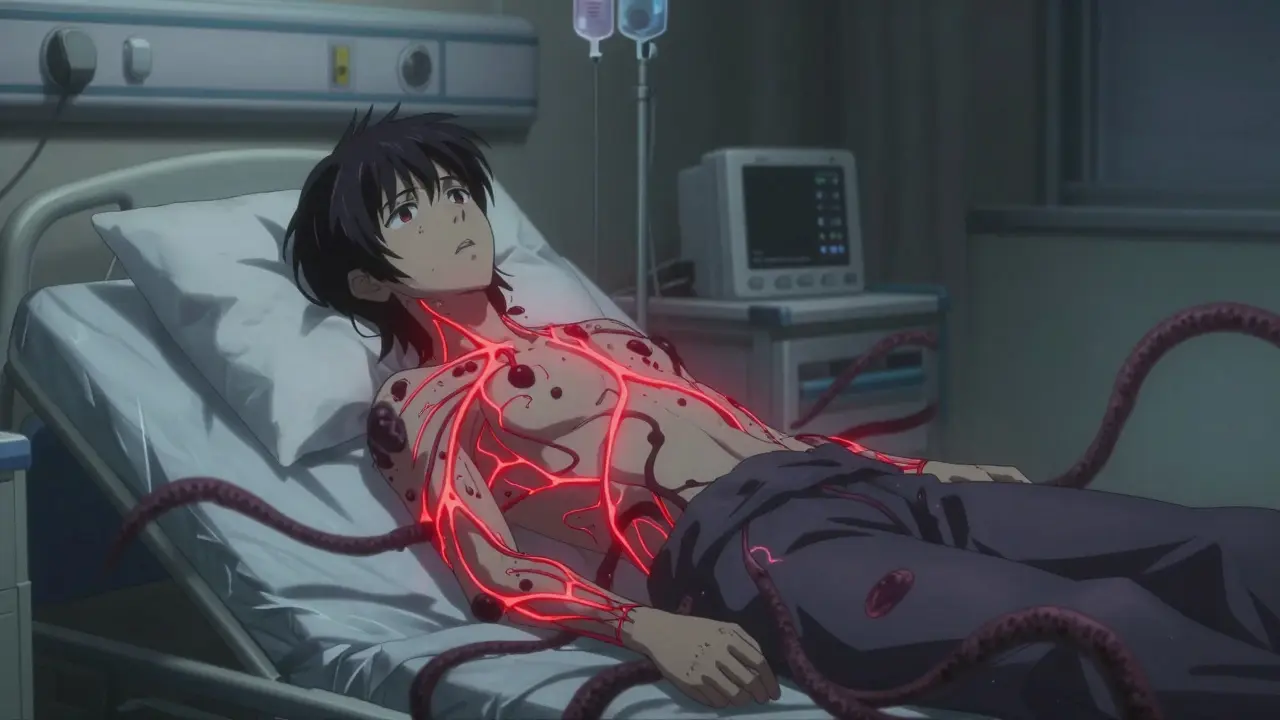
When your legs suddenly feel heavy, then your arms start to go numb, and you can’t even lift your head off the pillow - it’s not just fatigue. It’s not a pinched nerve. It’s something far more sudden, far more serious. This is Guillain-Barré Syndrome (GBS), a rare but dangerous autoimmune condition where your body’s own immune system turns on your peripheral nerves. Within days, what starts as tingling in your toes can become total paralysis. And if you don’t get treatment fast, you could stop breathing.
How GBS Attacks Your Nerves
GBS doesn’t come out of nowhere. It usually follows an infection - often a stomach bug caused by Campylobacter jejuni, a bacteria found in undercooked chicken or contaminated water. About one in five GBS cases links back to this bug. Other triggers include the flu, Epstein-Barr virus, Zika, and even rare reactions after surgery or vaccines. But here’s the twist: it’s not the infection itself that causes the damage. It’s your immune system’s overreaction. Mistaking nerve tissue for the invader, it launches an attack on the myelin sheath - the protective coating around your nerves. This slows or blocks the signals from your brain to your muscles. Result? Rapid, symmetrical weakness.
The weakness doesn’t stay put. It climbs. You start with numb feet, then weak ankles, then legs that won’t hold you up. Within days, your arms go limp. Half of patients lose control of their face - smiling becomes impossible, swallowing turns risky. In 20-30% of cases, the nerves controlling breathing fail. That’s when you’re rushed to the ICU. Without a ventilator, you can’t survive.
Why Time Is Everything
GBS doesn’t wait. Symptoms peak within 21 days, and 90% of patients hit their worst point by the end of the third week. But here’s the critical part: treatment works best if started within two weeks of the first symptoms. After that, the damage becomes harder to reverse. Every day you delay reduces the effectiveness of treatment by about 5%. That’s why doctors treat this like a code blue - even if the symptoms seem mild at first.
Diagnosis isn’t simple. GBS looks like other conditions - botulism, myasthenia gravis, even spinal cord compression. Doctors use three key tools: nerve conduction tests to measure how fast signals travel through nerves, a spinal tap to check for elevated protein in the cerebrospinal fluid (a hallmark of GBS), and a full neurological exam to confirm loss of reflexes. If you have ascending weakness, no reflexes, and no other explanation - it’s GBS.
IVIG: The First-Line Treatment
There are two main treatments for GBS: intravenous immunoglobulin (IVIG) and plasma exchange. But IVIG is now the go-to in most hospitals - and for good reason.
IVIG works by flooding your bloodstream with healthy antibodies from thousands of donors. These antibodies act like decoys. They distract your immune system from attacking your nerves. You get a dose every day for five days, usually through a standard IV in your arm. No central lines. No complex machines. Just a few hours in the hospital each day.
Studies show IVIG cuts recovery time by about half. Patients who get it walk independently about three weeks faster than those who don’t. Within two to four weeks, 60% of IVIG-treated patients show clear improvement. That’s compared to just 40% in untreated groups. For many, the first sign of progress? Wiggling a toe they couldn’t move before.
But it’s not magic. IVIG costs between $15,000 and $25,000 per course in the U.S. It’s not always available - global shortages hit hard during the pandemic. And it’s not safe for everyone. People with IgA deficiency can have life-threatening allergic reactions. Kidney problems? That’s another red flag. Side effects are common: headaches in 25% of patients, fever in 15%, and a small risk of blood clots.

IVIG vs. Plasma Exchange: What’s the Difference?
Plasma exchange, or plasmapheresis, removes your blood plasma - the part that contains the bad antibodies - and replaces it with donor plasma or albumin. It’s effective. Just as effective as IVIG in most studies. But it’s invasive. You need a central line. Each session takes hours. Complications like infections or low blood pressure happen in 30% of cases. IVIG? Only 15%.
Patients consistently report feeling better with IVIG. One Reddit user wrote: "The headaches during IVIG were brutal - felt like my skull was in a vice." But another said: "I got IVIG on day five. By day 12, I could wiggle my toes. No tubes in my neck. No scary machines. Just an IV.”
So why choose plasma exchange? Only in rare cases. If someone is crashing - rapidly losing lung function - some neurologists prefer plasma exchange because it clears antibodies faster. But the evidence is thin. For most, IVIG is safer, easier, and just as powerful.
What Doesn’t Work
Don’t expect steroids to help. Multiple high-quality trials have shown corticosteroids - like prednisone - have zero benefit in GBS. They don’t speed recovery. They don’t reduce disability. And they come with their own risks: high blood sugar, mood swings, bone loss. The Cochrane Review in 2017 summed it up: "No significant difference between steroids and placebo." So skip them. Don’t waste time.
What Happens After Treatment?
Recovery is slow. Even with IVIG, it takes months. Most people start to feel better within two to four weeks. But full recovery? That’s a different story. About 60% of patients regain full strength within six to twelve months. Another 30% have lasting weakness - maybe trouble climbing stairs, or needing a cane. And 10% remain severely disabled, unable to walk without help.
One patient on the GBS/CIDP Foundation forum shared: "I lost six months of my life. I couldn’t hold my baby. I needed a wheelchair. But I walked again. It took time. I had to relearn everything."
Autonomic instability is another hidden danger. Two-thirds of severe GBS cases involve wild swings in blood pressure, heart rate, or body temperature. That’s why ICU monitoring is non-negotiable. A sudden drop in heart rate? A spike in blood pressure? These can kill if not caught fast.

The Road Ahead
Research is moving forward. Scientists are now testing drugs that block the complement system - a key part of the immune attack in GBS. One drug, eculizumab, showed 30% faster recovery in early trials. Biomarkers like anti-ganglioside antibodies might soon help predict who responds best to IVIG. And in 2023, the FDA approved a subcutaneous immunoglobulin for CIDP - a chronic cousin of GBS. Could a similar option for GBS be next? Possibly.
But for now, IVIG remains the standard. It’s not perfect. It’s expensive. It’s not always available. But it saves lives. And for most people, it’s the difference between being trapped in a hospital bed and standing up again.
What You Need to Know Right Now
- If you or someone you know has sudden, spreading weakness - especially after an infection - get to a hospital immediately.
- Don’t wait for symptoms to get worse. GBS doesn’t wait.
- IVIG is the fastest, safest first-line treatment for most patients.
- Plasma exchange is an option, but it’s more invasive and not usually needed.
- Steroids don’t work. Don’t waste time on them.
- Recovery takes months. Patience and rehab are just as important as the initial treatment.
Can Guillain-Barré Syndrome come back?
It’s rare, but possible. About 5-10% of people who recover from GBS experience a relapse, usually within a few months. If weakness returns after initial improvement, it could be a different condition called chronic inflammatory demyelinating polyneuropathy (CIDP), which is treated differently. Always report any new symptoms to your neurologist.
Is IVIG safe for children with GBS?
Yes. IVIG is the standard treatment for children with GBS, and it’s just as effective as in adults. Dosing is based on weight - typically 0.4 grams per kilogram of body weight per day for five days. Children often recover faster than adults, but they still need close monitoring in the hospital, especially for breathing and heart issues.
Why does GBS cause pain?
Many people don’t realize GBS isn’t just weakness - it’s often extremely painful. Up to 80% of patients report deep aching, burning, or shooting pain in their limbs and back. This isn’t from muscle strain - it’s nerve damage. Pain management is a key part of treatment. Medications like gabapentin, pregabalin, or even low-dose antidepressants can help. Don’t ignore it - untreated pain slows recovery.
Can you get GBS from a vaccine?
It’s extremely rare. The risk is about 1-2 cases per million doses for vaccines like the flu shot. For comparison, you’re far more likely to get GBS from the flu itself. The CDC and WHO confirm that the benefits of vaccination far outweigh this tiny risk. No current vaccine has been linked to a significant increase in GBS cases.
How long does IVIG stay in your system?
IVIG lasts about 3 to 4 weeks in your bloodstream. That’s why it’s given as a 5-day course - to maintain a high enough level to calm the immune system. The effects on recovery, however, last much longer. The treatment doesn’t cure GBS - it interrupts the attack so your nerves can heal on their own over time.
What’s the survival rate for GBS?
With modern care, the survival rate is over 95%. Most deaths occur in people who aren’t treated quickly, especially if they develop respiratory failure without ventilation. Older adults and those with severe autonomic instability are at higher risk. But in a hospital with proper ICU support, GBS is rarely fatal.
What Comes Next?
If you’ve been through GBS, you’re not alone. Recovery is a marathon, not a sprint. Physical therapy, occupational therapy, and mental health support are just as vital as the IVIG. Many people need months of rehab to relearn how to walk, dress, or even swallow. Some return to work. Others adjust to a new normal. But most - 6 in 10 - get back to living fully.
GBS doesn’t define you. But how you respond to it - the speed of treatment, the patience in recovery, the support you accept - that does.

claire davies
December 24, 2025 AT 17:46Man, I remember when my cousin went through GBS after a nasty stomach bug. She was in the ICU for three weeks, hooked up to every machine under the sun. But the IVIG? It was like flipping a switch. One day she couldn’t lift her fingers, the next she was tracing letters on her notebook with her thumb. It’s wild how fast things can spiral - and how fast they can turn around if you catch it early. The pain part? Nobody talks about that enough. The burning in her legs felt like glass under her skin. Gabapentin saved her sanity. Honestly, if you’ve got sudden weakness after an infection, don’t wait for a second opinion. Just go. Now.
bharath vinay
December 25, 2025 AT 16:17Aurora Daisy
December 27, 2025 AT 05:02Andrea Di Candia
December 27, 2025 AT 14:20I’ve spent years studying autoimmune disorders, and what’s beautiful about GBS is how it reveals the body’s paradox - it’s trying to protect you, but it doesn’t know how to stop. The immune system isn’t evil. It’s confused. IVIG doesn’t suppress it. It whispers, ‘Hey, look over there - these antibodies are the real invaders.’ It’s not magic. It’s redirection. And yeah, it’s expensive. But so is a lifetime of paralysis. We spend billions on war. Why not spend a fraction to keep someone walking? We’re not just treating nerves. We’re restoring dignity.
John Pearce CP
December 29, 2025 AT 04:31Jillian Angus
December 31, 2025 AT 03:32CHETAN MANDLECHA
January 1, 2026 AT 18:49Ajay Sangani
January 3, 2026 AT 16:30Pankaj Chaudhary IPS
January 4, 2026 AT 00:38As a medical officer who has managed GBS cases in rural India, I can say with certainty that IVIG is a lifeline - if accessible. We’ve had patients recover from complete paralysis after receiving IVIG through NGO support. But the real tragedy isn’t the cost - it’s the delay. Families wait weeks because they don’t recognize the symptoms. We need community education. A simple poster in Hindi: ‘Tingling feet + weakness = Go to hospital NOW.’ That’s what saves lives. Treatment is effective. Awareness is the missing link.
Gray Dedoiko
January 5, 2026 AT 23:50Just want to say thank you for writing this. My sister got GBS after the flu last year. We thought it was just a bad cold. Took her 3 days to get into a hospital because the ER doc said ‘it’s probably just anxiety.’ She ended up on a ventilator. IVIG started on day 7. She’s walking again now, but still has nerve pain. I wish someone had told us earlier - like, yesterday - that this isn’t normal fatigue. Please, if you’re reading this and you’re a healthcare worker: trust the patient. If they say something’s wrong, even if it’s subtle, check for GBS.
Georgia Brach
January 6, 2026 AT 23:26Usha Sundar
January 7, 2026 AT 08:16Blow Job
January 8, 2026 AT 05:39My uncle had GBS. He’s 72. Got IVIG on day 5. By day 10, he was trying to stand. By day 20, he was walking with a cane. He said the worst part wasn’t the weakness - it was the silence. No one told him what to expect. He spent weeks wondering if he’d ever taste food again because his swallowing muscles were gone. He didn’t get rehab until month 3. That’s the real failure - not the treatment. It’s the lack of follow-up. Recovery isn’t just about the IV. It’s about the people who show up after the hospital lets you go.