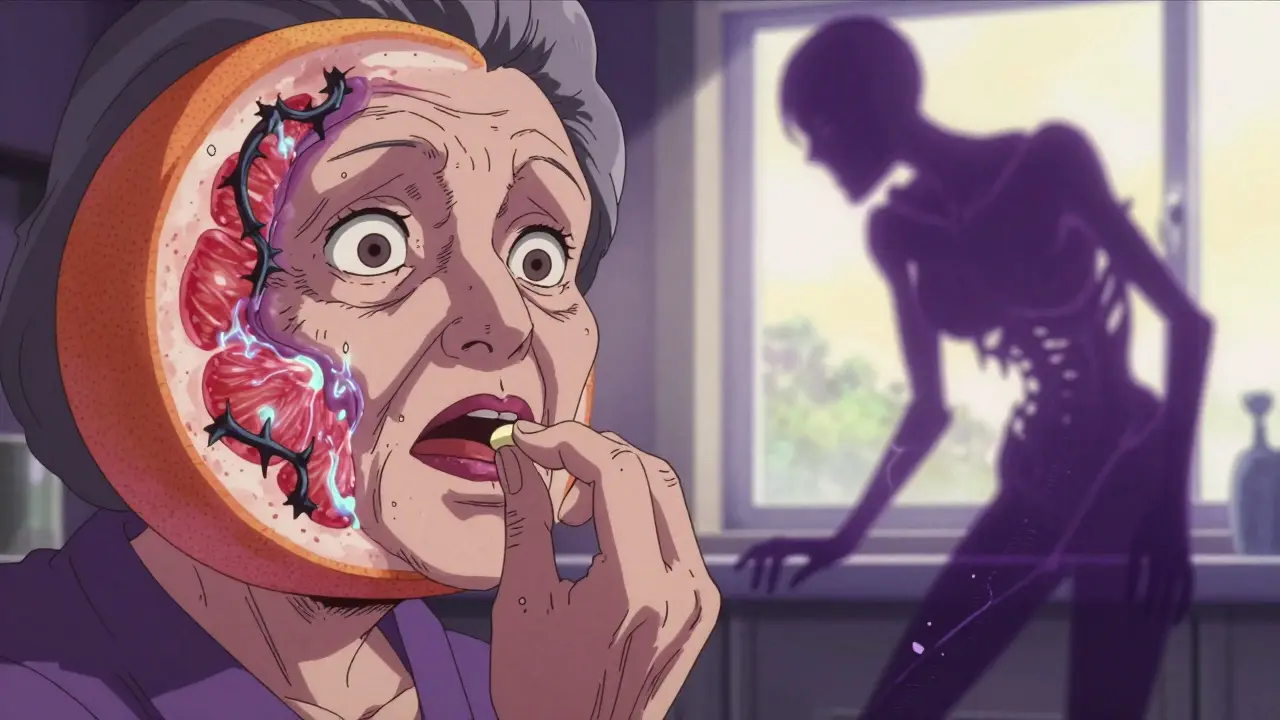
One glass of grapefruit juice in the morning might seem like a healthy start-until it turns into a silent danger if you're on certain medications. This isn’t a myth or an old wives’ tale. It’s science, and it’s life-threatening for some people. The problem isn’t the sugar or the acidity. It’s something hidden in the fruit that quietly changes how your body handles medicine. And once it happens, there’s no going back until your body rebuilds the enzymes it needs to process drugs properly.
How Grapefruit Juice Changes How Your Body Handles Medicine
Grapefruit juice doesn’t just mix with your pills-it rewires how they’re absorbed. The culprit? Furanocoumarins, natural chemicals found in grapefruit, especially bergamottin and 6',7'-dihydroxybergamottin. These compounds don’t just block a single enzyme. They permanently disable CYP3A4, a key enzyme in your small intestine that normally breaks down about half of all prescription drugs before they even enter your bloodstream.
When CYP3A4 is shut down, more of the drug slips through untouched. That means your body gets a much stronger dose than intended. For some medications, that’s the difference between a safe effect and a hospital visit. A single 250mL glass of grapefruit juice-about one small grapefruit-can boost the blood levels of felodipine (a blood pressure drug) by up to 800%. That’s not a typo. Eight times more drug in your system than your doctor prescribed.
And here’s the kicker: this effect lasts for days. Your body doesn’t just bounce back after you finish the juice. It takes about 72 hours for your intestines to make new CYP3A4 enzymes. So even if you drink grapefruit juice at breakfast and take your pill at dinner, you’re still at risk. Timing doesn’t fix this. Avoidance does.
Which Medications Are Most at Risk?
Not all medications are affected. But the ones that are? They’re often taken long-term-and by people who are most vulnerable: older adults, those on multiple drugs, or those with heart or liver conditions.
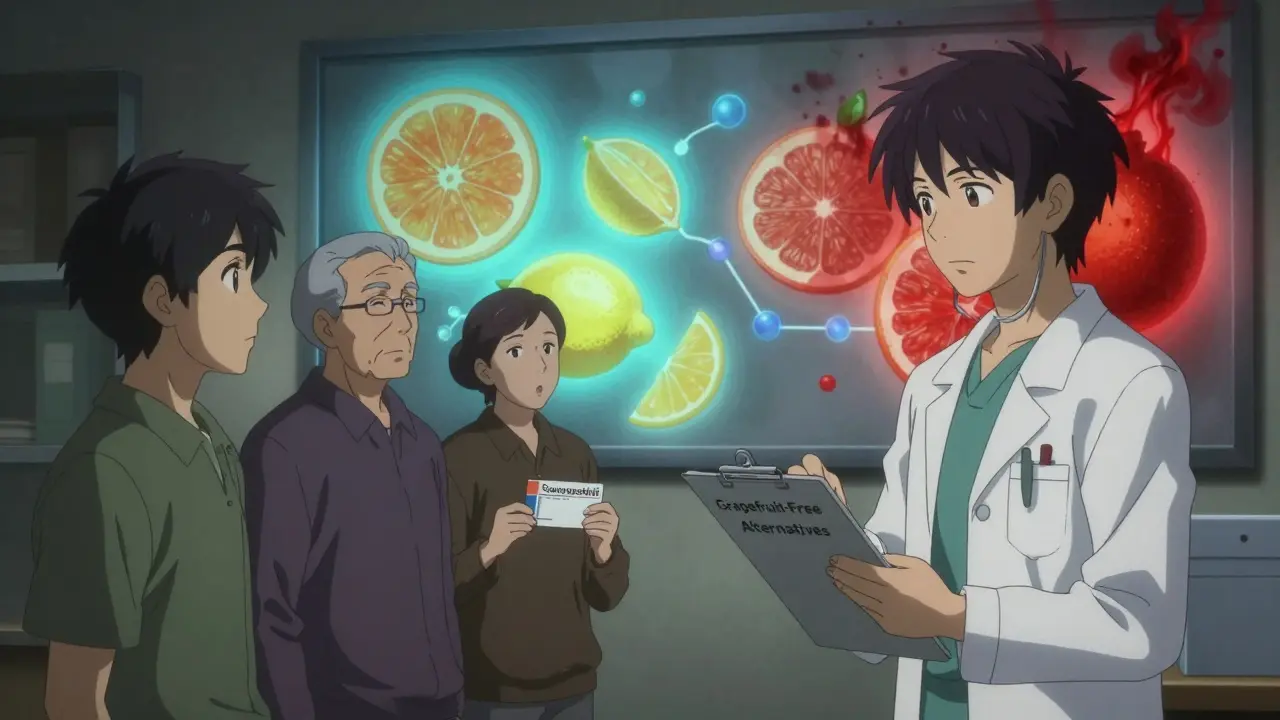
Statins are a major category. Simvastatin and lovastatin, used to lower cholesterol, see their blood levels jump by over 300% with grapefruit juice. That dramatically raises the risk of rhabdomyolysis-a condition where muscle tissue breaks down, flooding the kidneys with dangerous proteins. Atorvastatin is also risky, though less so. But pravastatin, rosuvastatin, and fluvastatin? They’re safe. They don’t rely on CYP3A4. If you’re on a statin and drink grapefruit juice, check which one you’re taking.
Blood pressure meds like felodipine, nifedipine, and verapamil are next on the list. Felodipine is one of the most dramatic examples. Amlodipine, however, is fine. Why? It’s metabolized differently. Same class, different pathway. That’s why you can’t assume all “calcium channel blockers” are equal.
Benzodiazepines like midazolam (used for sedation) and triazolam (a sleep aid) can cause excessive drowsiness or even breathing trouble. Immunosuppressants like cyclosporine and tacrolimus-critical for transplant patients-can become toxic, damaging kidneys or nerves. Antiarrhythmics like amiodarone can trigger dangerous heart rhythms. Even some antidepressants, like sertraline, have been flagged for potential interactions.
And then there are the surprises. Theophylline (for asthma) and itraconazole (an antifungal) actually drop in effectiveness with grapefruit juice. The reason? Grapefruit also blocks OATP transporters-proteins that help some drugs get absorbed. So sometimes, it’s not too much drug-it’s too little.
It’s Not Just Juice-It’s the Whole Fruit, and Other Citrus Too
Some people think they’re safe if they eat the fruit instead of drinking juice. Wrong. The same furanocoumarins are in the pulp, peel, and segments. One whole grapefruit has the same effect as a glass of juice. Frozen concentrate? Same thing. Even freshly squeezed from your countertop juicer? Still dangerous.
And it’s not just grapefruit. Seville oranges-used in traditional marmalade-contain nearly identical levels of furanocoumarins. Pomelos, a larger cousin of grapefruit, are just as risky. If you’re on a high-risk medication, skip them too.
But regular oranges, tangerines, and clementines? Safe. They don’t contain the same chemicals. Lemons and limes? Also safe in normal amounts. You don’t need to give up citrus entirely-just the ones that can hurt you.
Why Some People Are More Affected Than Others
Not everyone reacts the same way. One study showed that when 10 people drank the same grapefruit juice with the same dose of felodipine, drug levels increased anywhere from 0% to 800%. Why? Because people have different baseline levels of CYP3A4 in their intestines. Some naturally have more-so when it’s blocked, the impact is bigger.
Genetics play a role too. A variant called CYP3A4*22 is linked to higher interaction risk. Older adults are more vulnerable because they often take more medications and their bodies process drugs slower. Liver or kidney disease? That adds another layer of risk. Even your gut health can influence how much of the enzyme is present.
That’s why blanket advice like “just avoid it” is the only safe rule. You can’t test yourself. You can’t guess your risk. And if you’re on multiple meds, the chances you’re taking one affected by grapefruit? They’re high. About 42% of adults over 40 in the U.S. take at least one medication that interacts with grapefruit juice. That number is likely similar in the UK.
What Doctors and Pharmacists Are Doing About It
For years, this was an under-the-radar issue. But now, it’s front and center. The FDA requires grapefruit interaction warnings on 21 high-risk medications, including simvastatin, felodipine, and cyclosporine. About 19% of all prescription labels in the U.S. now carry that warning-up from 12% in 2015.
Electronic health records now flag grapefruit interactions automatically. Pharmacies use software that checks every new prescription against a database of over 85 known interactions. The European Medicines Agency estimates grapefruit-related adverse events cause 85 serious incidents and 12 deaths per year in the EU alone.
But here’s the gap: education still falls short. Only 37% of pharmacists consistently warn patients. And only 28% of patients can correctly name the medications they should avoid with grapefruit-even after being told. Many assume the warning doesn’t apply to them. Or they forget. Or they think “a little won’t hurt.”
That’s why the American Pharmacists Association launched a ‘Grapefruit-Free Alternatives’ program in 2020. It’s helped over 14,000 patients switch to safer versions of their meds. For example, switching from simvastatin to rosuvastatin removes the risk entirely. No lifestyle change needed-just a different pill.
What You Should Do Right Now
If you take any prescription medication, here’s what to do:
- Check your labels. Look for “do not take with grapefruit juice” or “avoid grapefruit products.” If it’s not there, ask your pharmacist.
- Make a list. Write down every medication you take-prescription, over-the-counter, even supplements. Bring it to your pharmacist. They can cross-check it in seconds.
- Ask about alternatives. If you’re on simvastatin, ask if pravastatin or rosuvastatin is an option. If you’re on felodipine, ask about amlodipine. Many safer alternatives exist.
- Be consistent. If you’re told to avoid grapefruit, avoid it completely. No exceptions. Not even once a week. The enzyme damage is cumulative and lasts three days.
- Teach someone. If you live with family or a caregiver, make sure they know too. Accidental consumption is a common cause of hospital visits.
And if you’re not sure? Don’t guess. Call your pharmacy. Or use the NHS online medicines checker. Better safe than sorry.
The Future: Can We Fix This?
Scientists are working on solutions. Researchers at the University of Florida are using CRISPR gene editing to create furanocoumarin-free grapefruit. Early trials are promising. If successful, we might one day enjoy grapefruit without fear.
Meanwhile, new tools are emerging. The FDA is considering routine CYP3A4 testing for high-risk patients-a way to predict who’s most vulnerable. And some drug manufacturers are reformulating pills to reduce interaction risk. For example, extended-release felodipine causes a smaller spike than the immediate-release version.
But until then, the rule remains simple: if your medication has a grapefruit warning, don’t take it with grapefruit. Not even a sip. Not even once. Because the damage isn’t just theoretical. It’s real. And it’s happened before.
Can I drink grapefruit juice if I take my medication at night?
No. Grapefruit juice disables intestinal enzymes for up to 72 hours. Even if you take your medication at night and drink juice in the morning, the enzymes are still blocked. The timing doesn’t matter-only the presence of the juice. Avoid it entirely if your drug is affected.
Is orange juice safe to drink with my medications?
Yes. Regular oranges, tangerines, and clementines do not contain furanocoumarins and are safe to consume with medications. However, Seville oranges (used in marmalade) and pomelos are not safe-they have the same harmful compounds as grapefruit.
What if I accidentally drank grapefruit juice with my medication?
If it’s a one-time incident and you feel fine, monitor yourself for unusual side effects like muscle pain, dizziness, irregular heartbeat, or extreme drowsiness. Contact your pharmacist or doctor if you’re concerned. Don’t panic-but don’t ignore it. Avoid grapefruit completely going forward.
Are there any medications that are completely safe with grapefruit?
Yes. Many medications aren’t affected. Examples include pravastatin, rosuvastatin, fluvastatin, amlodipine, losartan, and levothyroxine. But you can’t assume-always check with your pharmacist. Even within the same drug class, some versions are safe and others aren’t.
Why don’t all doctors warn patients about grapefruit interactions?
Many doctors don’t realize how common or serious these interactions are. Studies show only 37% of pharmacists consistently counsel patients. The information isn’t always clear on labels, and the number of affected drugs keeps growing. That’s why it’s up to you to ask-especially if you’re over 40 or take multiple medications.


christy lianto
January 8, 2026 AT 06:57Just found out my mom’s on simvastatin and drinks grapefruit juice every morning. I’m calling her right now. This post saved a life.
Luke Crump
January 9, 2026 AT 04:59So let me get this straight-nature invented a fruit that sabotages modern medicine, and we’re supposed to be grateful? This is evolution’s middle finger to pharmacists. We’re not meant to live this long anyway.
Annette Robinson
January 10, 2026 AT 04:58I’m a pharmacist, and I see this every single day. Patients say, ‘But I’ve been drinking it for years!’ and I have to gently explain that ‘years’ doesn’t mean ‘safe.’ One patient ended up in ICU because she thought ‘a little bit’ wouldn’t hurt. It did. Please, if you’re on meds-just say no. It’s not worth the gamble.
Ken Porter
January 10, 2026 AT 16:11Why are we letting a fruit dictate our healthcare? This is why America’s medical system is broken. If you can’t handle a grapefruit, maybe you shouldn’t be on pills.
swati Thounaojam
January 10, 2026 AT 16:20i never knew this! my dad takes blood pressure med and he loves grapefruit. gonna tell him now. thank u!!
Evan Smith
January 12, 2026 AT 06:23Wait, so if I drink grapefruit juice at 7am and take my pill at 8pm… I’m still screwed? That’s wild. So the real enemy isn’t the pill-it’s the juice’s revenge. I’m just here for the drama.
Lois Li
January 13, 2026 AT 00:08Thank you for writing this so clearly. I shared it with my book club-most of us are over 50 and on at least three meds. We’re all switching to orange juice now. And yes, I double-checked the label on my statin. Turns out I’m on rosuvastatin. Phew.
Kristina Felixita
January 14, 2026 AT 18:26OMG!! I just realized I’ve been drinking grapefruit juice with my cyclosporine since my transplant… I’m so scared right now!! I’m calling my doctor NOW!! Thank you for posting this!!
Joanna Brancewicz
January 15, 2026 AT 02:40CYP3A4 inhibition via furanocoumarins is a well-documented pharmacokinetic interaction. The half-life of enzyme regeneration is ~72h. Avoidance is the only evidence-based intervention.
Manish Kumar
January 17, 2026 AT 00:41You know, this whole grapefruit thing makes me think about how deeply we’ve severed our connection with nature. We used to live with the rhythms of the earth, but now we’re terrified of a fruit because we’ve built a medical system that’s fragile as glass. Is it the grapefruit that’s dangerous-or the fact that we’ve outsourced our bodies to chemistry? Maybe we should ask: Why do we need so many drugs in the first place?
Aubrey Mallory
January 18, 2026 AT 17:14People still don’t get it. This isn’t about ‘maybe’ or ‘sometimes.’ It’s about absolute zero tolerance. If your doctor didn’t warn you, they’re lazy. If you ignored it, you’re reckless. No more excuses.
Dave Old-Wolf
January 19, 2026 AT 17:30My grandma took felodipine and drank grapefruit juice every day for 10 years. She never had a problem. So maybe it’s not as bad as they say? Or maybe she just got lucky?
Prakash Sharma
January 21, 2026 AT 12:37In India, we don’t even have grapefruit juice. We have jamun and amla-natural, safe, and better for you. Why are Americans so obsessed with this fruit? Maybe we should export our wisdom instead of importing problems.