Gut Absorption Estimator
How Your Gut Affects Medication Absorption
Based on the article "Gastrointestinal Medications: Why Absorption Problems Reduce Effectiveness"
Enter your details above and click "Calculate Absorption" to see estimated effectiveness
Important: This tool provides general estimates based on clinical studies. Your actual absorption may vary. Always consult your healthcare provider about medication effectiveness.
Most people assume that if you swallow a pill, it will work as expected. But for many gastrointestinal medications, that’s not true. Even when taken exactly as prescribed, drugs like levothyroxine, mesalamine, or warfarin often fail to reach the right levels in the blood. Why? Because the gut isn’t just a tube-it’s a complex, changing environment that can block, slow, or destroy drugs before they ever get into your system.
How Your Gut Blocks Medications
Your small intestine has a surface area bigger than a tennis court, thanks to millions of tiny finger-like projections called villi. That sounds like a good thing for absorbing drugs, right? But the same structures that help nutrients enter your body also act as gatekeepers. The intestinal lining has tight junctions, a thick mucus layer, and powerful pump proteins like P-glycoprotein that actively push drugs back out. These barriers exist to keep toxins out-but they also keep many medicines out.Drugs that are too large (over 500 Daltons), too water-soluble, or too polar struggle to pass through. Insulin, for example, is a protein with a molecular weight of over 5,800 Daltons. If you swallow it, almost none of it gets absorbed-less than 1%. That’s why insulin has to be injected. The same problem affects many newer drugs being developed for chronic conditions, especially biologics.
Then there’s the pH gradient. Your stomach is acidic, around pH 2, but by the time you reach the lower small intestine, it’s nearly neutral at pH 8. Many drugs dissolve better in one pH than another. If a drug is designed to dissolve in the stomach but your stomach empties too slowly, or if it’s meant to release in the intestine but your gut pH is off due to acid-reducing meds, absorption drops. A pill that works perfectly in a healthy person might barely register in someone with Crohn’s disease or GERD.
Food, Timing, and the Hidden Rules of Absorption
You’ve probably been told to take some meds on an empty stomach. That’s not just a suggestion-it’s often the difference between the drug working and not working at all.Levothyroxine, used for hypothyroidism, is a classic example. If you take it with coffee, calcium supplements, or even a bowl of oatmeal, absorption can drop by 30-50%. That’s why doctors insist on taking it first thing in the morning, at least 30-60 minutes before eating. The reason? Food slows gastric emptying by 2 to 4 hours. Your stomach sits there, holding the pill, while the drug waits for the right conditions to be absorbed.
Fatty meals are especially tricky. They trigger bile release and slow gut movement, which can delay or reduce absorption of fat-soluble drugs. Antibiotics like tetracycline bind to calcium in dairy products, making them useless. Even something as simple as grapefruit juice can interfere with how your liver processes certain medications, increasing the risk of side effects.

Disease Changes Everything
If you have inflammatory bowel disease (IBD), short bowel syndrome, or even long-term constipation, your body doesn’t process drugs the same way as someone with a healthy gut.In ulcerative colitis, the inflammation in the colon can destroy the very cells that absorb drugs. Studies show that patients with active disease absorb 25-40% less of immediate-release mesalamine compared to healthy people. That means their medication isn’t working-not because they’re noncompliant, but because their gut can’t hold onto it.
Patients with short bowel syndrome have lost so much of their small intestine that there’s simply not enough surface area left for absorption. Some need two to three times the normal dose of antibiotics or vitamins just to reach therapeutic levels. Others find that extended-release pills don’t work at all-the drug passes through before it has time to release.
And then there’s the issue of motility. Drugs like semaglutide (used for diabetes and weight loss) slow down gut movement. That’s good for blood sugar control, but bad for other pills you’re taking. A patient on semaglutide might find their blood thinner isn’t working as well because the drug is sitting in the stomach too long, or moving too slowly through the intestine. Pharmacists report INR levels swinging wildly in IBD patients on warfarin-sometimes therapeutic, sometimes dangerously high-all without changing the dose.
Formulation Matters More Than You Think
Not all pills are created equal. The same active ingredient can behave completely differently depending on how it’s made.Take mesalamine again. Some versions are designed to dissolve in the colon (like Asacol HD). But if a patient has severe inflammation, the colon is too damaged to absorb the drug properly. The medication might dissolve too early or too late, missing the target entirely. In these cases, a different formulation-like a suppository or enema-works better.
Some drugs are made as salts or crystals to dissolve faster. Others are coated to survive stomach acid. A poorly formulated version might sit in the gut for hours without dissolving, while a better one releases its payload in under 30 minutes. That’s why generic versions don’t always work the same way as brand-name drugs, especially for medications with narrow therapeutic windows.
There’s also a growing field of absorption enhancers. Sodium caprate, chitosan, and medium-chain fatty acids can temporarily open tight junctions in the gut lining, letting drugs slip through more easily. These are already being used in some newer formulations to boost bioavailability. One study showed a 200% increase in absorption for certain drugs using these enhancers.
What You Can Do About It
If you’re on a gastrointestinal medication and it doesn’t seem to be working, don’t assume it’s your fault. Talk to your doctor or pharmacist. Ask:- Should I take this on an empty stomach?
- Are there foods, supplements, or drinks I should avoid?
- Is there a different formulation that might work better for me?
- Could my condition be affecting how the drug is absorbed?
For patients with chronic GI conditions, specialized formulations are often the answer. Liquid suspensions, chewable tablets, or even transdermal patches can bypass the gut entirely. In children under 8, swallowing pills is hard-oral suspensions are essential. For adults with swallowing issues, crushing pills isn’t always safe. Some are designed to release slowly, and crushing them can cause dangerous spikes in blood levels.
Even something as simple as timing matters. Taking your thyroid medication at night instead of in the morning might seem like a small change, but it can throw off your entire hormone balance. Always follow the instructions exactly-and if you can’t, ask why.
The Future Is Personalized
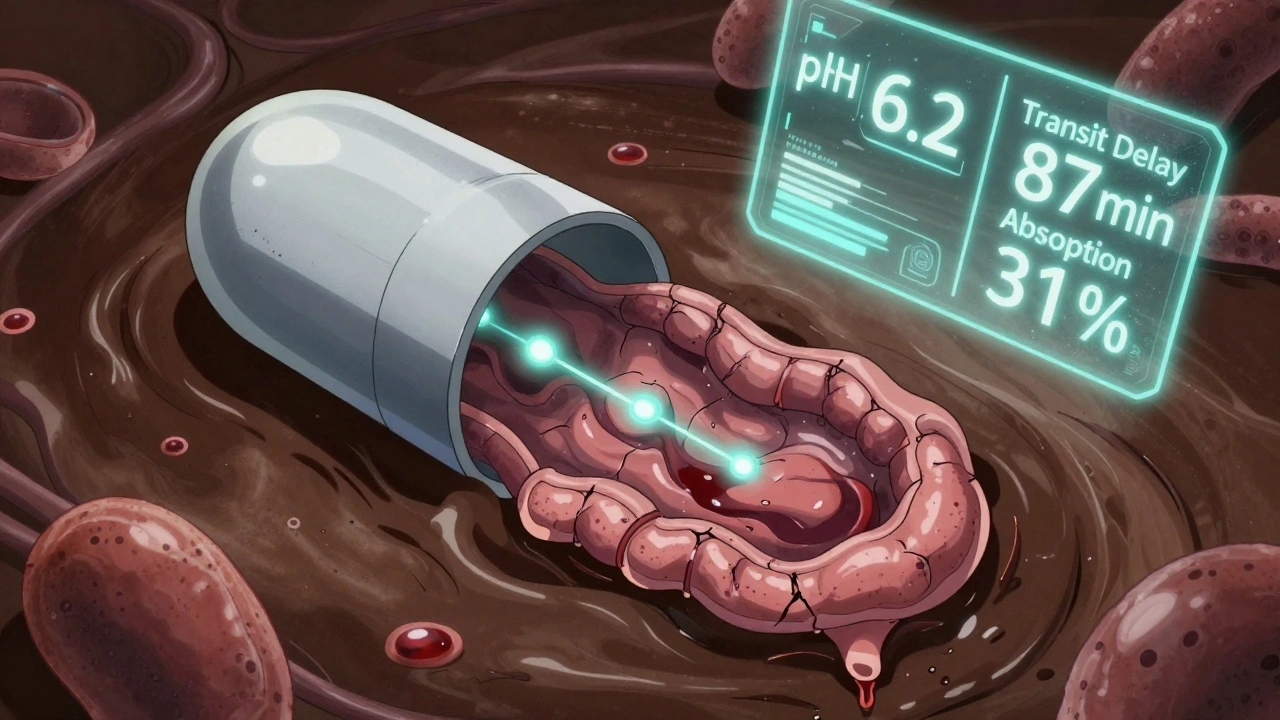
Researchers are now building computer models that simulate how drugs move through a diseased gut. These models, called PBPK (physiologically based pharmacokinetic) models, can predict how a drug will behave in someone with Crohn’s, IBS, or post-surgical changes. In the next five years, we’ll likely see pills with built-in sensors that track pH, pressure, and transit time in real time. Imagine a capsule that tells your phone: "I’ve reached your jejunum, but your mucus layer is thicker than normal-I’ll release the drug in 20 minutes."Pharmaceutical companies are investing heavily in this. The global market for absorption enhancers is expected to grow from $1.2 billion in 2022 to $2.8 billion by 2027. And regulatory agencies like the FDA now require drug makers to test their products in models that mimic disease states-not just healthy guts.
But until then, the best tool you have is awareness. If your medication isn’t working, it’s not just about dosage. It’s about how your body handles it. The gut is a master negotiator. It decides what gets in, what gets out, and when. Understanding that can save you from ineffective treatment, dangerous side effects, and unnecessary frustration.
Why do some GI medications stop working even if I take them regularly?
Many gastrointestinal medications rely on specific conditions in the gut to be absorbed properly. If you have inflammation, slowed motility, altered pH, or damage to the intestinal lining-common in conditions like Crohn’s or ulcerative colitis-your body may not absorb the drug as expected. Even small changes in food intake, timing, or other medications can interfere. It’s not about compliance; it’s about physiology.
Can I crush my pills if I have trouble swallowing them?
Only if the label says it’s safe. Many GI medications are designed with special coatings or time-release mechanisms. Crushing them can destroy those systems, causing too much drug to be released at once (risking side effects) or none at all (making it ineffective). Always check with your pharmacist before altering the form of any medication.
Why does my doctor tell me to take levothyroxine on an empty stomach?
Levothyroxine is easily blocked by food, calcium, iron, and even coffee. These substances bind to the hormone in the gut and prevent absorption. Taking it on an empty stomach ensures maximum uptake. Waiting 30-60 minutes before eating gives your body time to absorb it before anything interferes.
Do generic versions of GI drugs work the same as brand names?
For many drugs, yes. But for medications with narrow therapeutic windows-like warfarin, levothyroxine, or seizure drugs-small differences in formulation can matter. Generic versions may dissolve at different rates or use different inactive ingredients that affect absorption. If you switch generics and notice changes in how you feel, tell your doctor. You may need to stick with one brand.
Are there new treatments that help GI medications absorb better?
Yes. New formulations use absorption enhancers like sodium caprate or chitosan to temporarily open gaps in the gut lining. Nanoparticles and liposomes are also being developed to protect drugs from digestion and carry them directly to absorption sites. These are mostly in clinical trials now, but they’re already changing how drugs like insulin and biologics are delivered.


Brooke Evers
December 7, 2025 AT 06:24I’ve been on levothyroxine for six years and I used to think I was just bad at remembering to take it on an empty stomach. Turns out, my morning coffee was sabotaging me the whole time. I switched to tea and started taking it right when I woke up, no food, no supplements - and my TSH dropped from 7.2 to 2.8 in three months. It’s wild how something so small can make or break your treatment. I wish more doctors talked about this stuff instead of just saying ‘take your meds.’
Chris Park
December 7, 2025 AT 21:54Let’s be real - this whole ‘gut absorption’ narrative is corporate propaganda. The pharmaceutical industry doesn’t want you to know that most of these drugs are designed to fail so you’ll keep buying them. Why do you think they patent formulations that only work under perfect conditions? They know most people can’t follow the 30-minute fasting rule, so they profit from your ‘noncompliance.’ The real solution? Stop trusting pills. Eat real food. Detox your liver. The body heals itself - if you stop poisoning it with synthetic chemicals.
Inna Borovik
December 8, 2025 AT 22:35While I appreciate the clinical breakdown, the post ignores a critical variable: microbiome variability. Recent studies (2023, Gut Journal) show that gut flora composition directly alters drug metabolism - particularly for warfarin and mesalamine. A patient with high Bacteroidetes might metabolize a drug 40% faster than someone with dominant Firmicutes. This isn’t just about pH or motility - it’s about microbial enzymes breaking down or activating compounds before absorption. Yet no pill comes with a microbiome compatibility label. We’re treating biology like a fixed system when it’s a dynamic ecosystem.
Rashmi Gupta
December 9, 2025 AT 15:07So what you’re saying is… the whole system is rigged? I’ve been on 3 different generics of levothyroxine and each time I switched, I felt like I was drowning in fatigue. My doctor just shrugged and said ‘it’s the same molecule.’ But my body knew. It knew the difference. And now I’m stuck paying $80 a month for the one brand that doesn’t make me want to sleep for a week. Why does my body have to be the lab test for Big Pharma’s lazy formulations?
brenda olvera
December 10, 2025 AT 03:43I’m so glad someone finally said this out loud. I have Crohn’s and I used to feel so guilty when my meds didn’t work. Like I was doing something wrong. But it’s not me - it’s my gut. I switched to an enema for my mesalamine and it’s been a game changer. No more bloating, no more crashes. I wish I’d known sooner. To anyone out there feeling hopeless - talk to your pharmacist. They know the hacks. You’re not broken. Your body just needs a different key.
Myles White
December 10, 2025 AT 06:15This is such an important topic and I’ve seen it firsthand with my dad who had short bowel syndrome after resection. He was on vitamin B12 injections because oral supplements did absolutely nothing - even high-dose ones. His body just couldn’t hold onto anything. We tried liquid formulations, chewables, even sublinguals. Only the injections worked. And now he’s on a custom compounded version of his blood thinner that’s designed to release over 8 hours instead of 12. It’s not just about the drug - it’s about how it’s delivered. The future of medicine isn’t one-size-fits-all. It’s one-size-fits-one. And that’s actually kind of beautiful.
Nigel ntini
December 11, 2025 AT 01:34I’ve worked as a pharmacist for 18 years and I can tell you - the biggest issue isn’t the gut. It’s the lack of communication between prescribers and patients. Most people don’t know what ‘take on empty stomach’ really means. They think it’s just ‘no breakfast.’ But what about that almond milk latte? The calcium supplement they took at lunch? The grapefruit they ate yesterday? We need better patient education - not just pamphlets, but videos, voice notes, even text reminders. And we need pharmacists involved from day one, not just when the prescription runs out.
Mansi Bansal
December 12, 2025 AT 14:07It is an incontrovertible fact that the modern pharmaceutical paradigm has systematically neglected the physiological heterogeneity of the human gastrointestinal tract. The reductionist model of drug absorption, predicated upon the assumption of a homogenous, healthy enteric environment, is not merely inadequate - it is epistemologically flawed. One cannot prescribe a single pharmacokinetic protocol to individuals exhibiting divergent mucosal integrity, microbial colonization patterns, and motility indices without invoking a profound ethical lapse. The current standard of care is not medicine - it is statistical tyranny.
pallavi khushwani
December 13, 2025 AT 15:06you know what’s wild? the body knows what it needs. i used to take my thyroid med at night because i forgot in the morning. then i started feeling like a zombie. switched to morning - felt human again. no lab test told me that. my body did. maybe the real science isn’t in the pill… it’s in listening. we’ve forgotten how to listen to ourselves. we outsource our health to doctors and drugs and forget we’re alive. just a thought.
Dan Cole
December 13, 2025 AT 23:15Let me cut through the fluff. The entire pharmaceutical industry is built on obscurity. They design drugs to be absorbed only under perfect conditions - conditions that 98% of people can’t maintain - so they can sell you more pills, more tests, more ‘special formulations.’ They know grapefruit interferes. They know coffee blocks absorption. They know your gut is broken from years of processed food. But they don’t fix the system. They monetize the failure. And now they’re selling ‘smart pills’ with sensors - because why fix absorption when you can charge $500 for a pill that texts your phone? This isn’t innovation. It’s extortion with a patent.