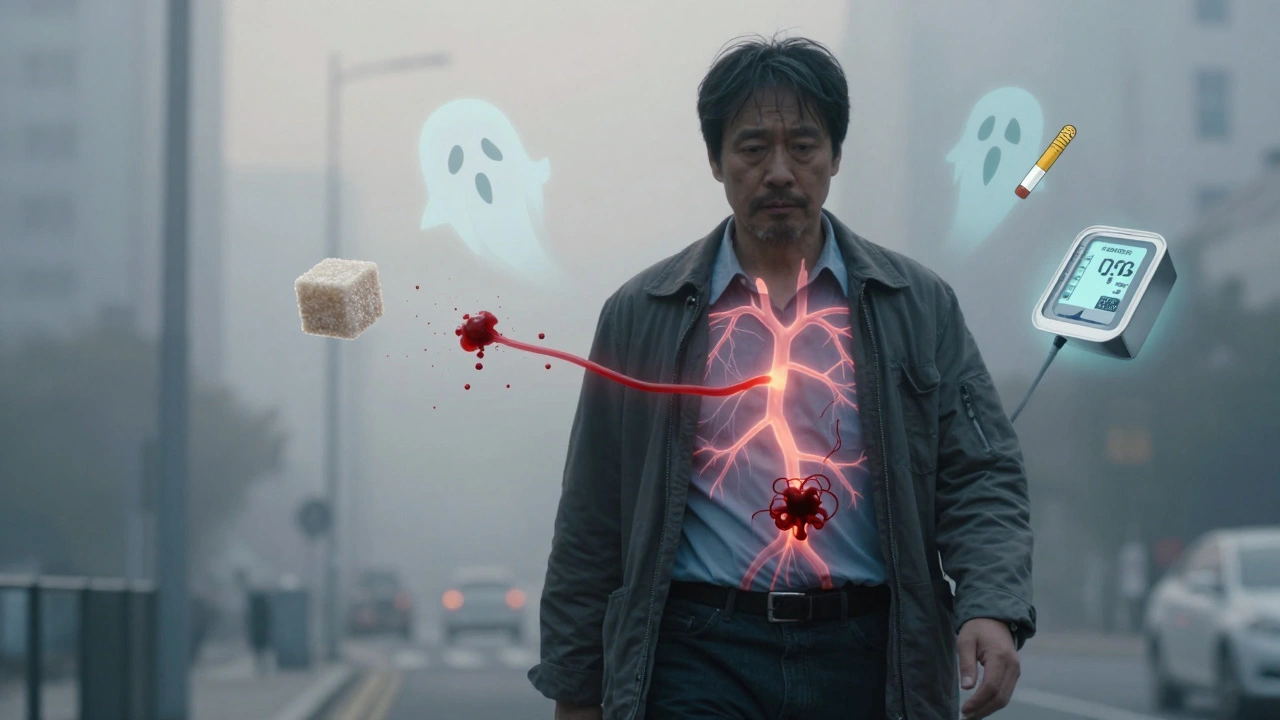
Coronary artery disease isn’t just a buzzword in medical reports-it’s the number one killer worldwide. If you’ve ever heard someone say, "He had a heart attack out of nowhere," chances are, underlying atherosclerosis was quietly building for years. This isn’t about bad luck. It’s about what happens inside your arteries over time-and how you can stop it before it’s too late.
What Exactly Is Atherosclerosis?
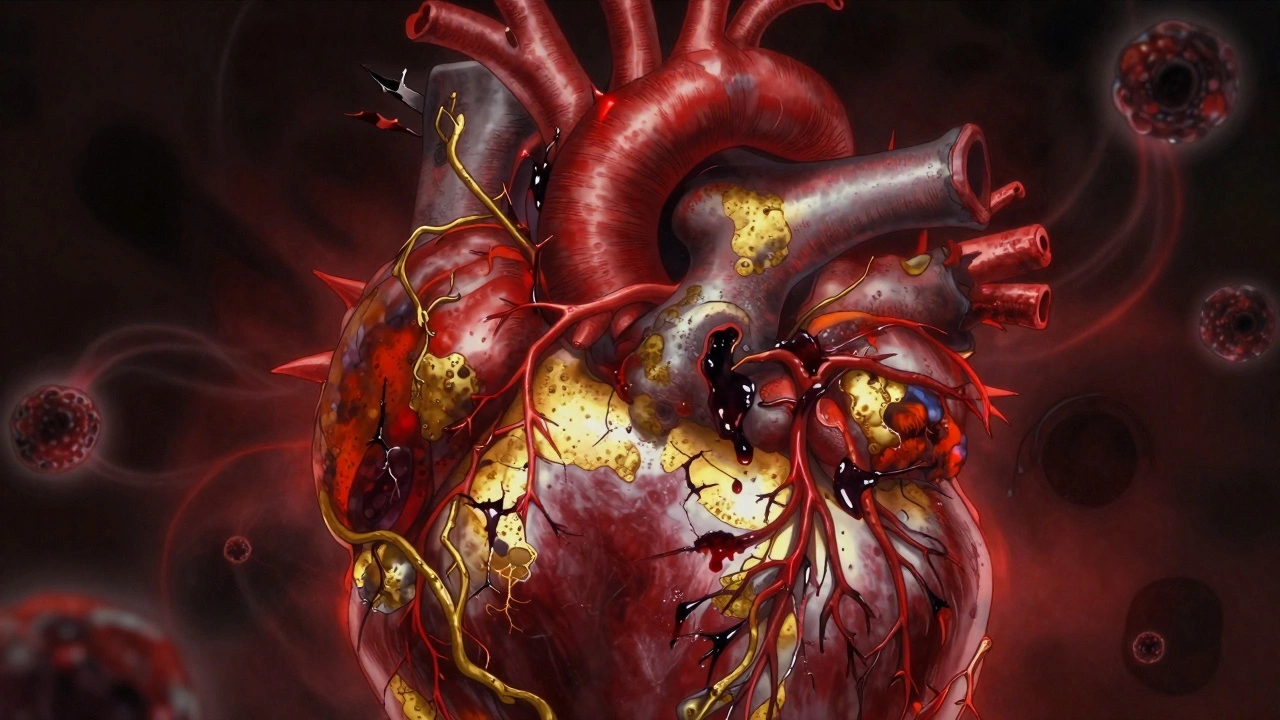
Atherosclerosis is the silent architect behind most heart attacks. It starts when fatty deposits-mostly cholesterol, calcium, and cellular waste-clump together inside the walls of your coronary arteries. These aren’t just blobs of fat. They’re complex structures called plaques. Over time, they harden, narrow the artery, and restrict blood flow to your heart muscle. Not all plaques are the same. Some grow slowly and cause a steady narrowing-often more than 50%-leading to predictable chest pain during exercise. These are called stable plaques. Others are dangerous because they look almost harmless on scans. They’re soft, rich in fat, and have a thin outer layer. These unstable plaques may only block 30% of the artery, but they’re ticking time bombs. They can rupture suddenly, triggering a blood clot that completely blocks the artery-and that’s when a heart attack happens. This is why a person can have a heart attack even if their last stress test looked fine. The real danger isn’t always the blockage size. It’s the plaque’s makeup.Who’s at Risk? The Real Culprits Behind CAD
You can’t change your age or genetics, but you can control most of what drives coronary artery disease. The biggest risk factors aren’t what you think.- High LDL cholesterol-the "bad" kind-is the main fuel for plaque. When LDL particles slip into artery walls, they trigger inflammation. Your body sends immune cells to clean up the mess, but instead, they get trapped and turn into foam cells that swell the plaque.
- Smoking damages the inner lining of arteries, making it easier for cholesterol to stick. It also makes blood more likely to clot. Even secondhand smoke raises your risk.
- High blood pressure puts constant stress on artery walls. Over time, this weakens them and speeds up plaque buildup.
- Diabetes doesn’t just affect blood sugar. It changes how your body handles fat and inflammation, making plaques more unstable and harder to treat.
- Obesity, especially belly fat, releases hormones that raise blood pressure, insulin resistance, and inflammation-all of which feed atherosclerosis.
- Family history matters, but not as much as you might fear. If a close relative had heart disease before 55 (men) or 65 (women), your risk goes up. But lifestyle can still override this.
How Is It Diagnosed? Beyond the Chest Pain
Many people think a heart attack is the first sign of coronary artery disease. But by then, it’s often too late. The real goal is catching it before symptoms hit.- Electrocardiogram (ECG) is the first test. It measures your heart’s electrical activity. If you’ve had a past heart attack or are having chest pain, it can show signs of damage or reduced blood flow.
- Stress tests watch how your heart performs under physical strain. You walk on a treadmill while your heart rhythm, blood pressure, and breathing are monitored. If your heart doesn’t get enough oxygen during exercise, it shows up on the test.
- Coronary angiography is the gold standard. A thin tube is threaded into your artery, dye is injected, and X-rays show exactly where blockages are. It’s invasive, but it gives the clearest picture.
- CT calcium scans detect calcium in artery walls-a sign of long-term plaque buildup. A high score means more risk, even if you feel fine.
- Ankle-Brachial Index (ABI) checks for blocked arteries in your legs. If you have peripheral artery disease, you almost certainly have coronary artery disease too.
Treatment: It’s Not Just Pills
There’s no magic pill that erases plaque. But you can stabilize it, slow it down, and prevent it from killing you. Lifestyle changes are the foundation. No drug works as well as quitting smoking, eating real food, and moving daily. A Mediterranean-style diet-rich in vegetables, fish, nuts, olive oil, and whole grains-lowers LDL and reduces inflammation better than any statin alone. Medications are essential for most people. Here’s what’s proven:- Statins lower LDL cholesterol by up to 50%. They also stabilize plaques, making them less likely to rupture. Most people with CAD need them for life.
- Aspirin or other antiplatelets prevent clots from forming on plaques. Not everyone needs them-only those with a history of heart attack, stent, or bypass.
- ACE inhibitors or ARBs lower blood pressure and reduce strain on the heart, especially if you’ve had a heart attack or have heart failure.
- Beta-blockers slow your heart rate and lower blood pressure. They’re often used after a heart attack to reduce future risk.
- SGLT2 inhibitors and GLP-1 agonists were originally for diabetes, but studies now show they cut heart attack and death risk even in people without diabetes.
The New Frontier: Personalized Care and Cardio-Oncology
The 2023 guidelines changed everything. Doctors now don’t just treat your cholesterol number. They assess your total risk: age, sex, diabetes, kidney function, smoking history, and even how many arteries are affected. If your risk is low-under 1% per year-you might only need lifestyle changes and a statin. If you’re high risk-over 3% per year-you’ll likely need multiple medications, aggressive LDL targets (under 55 mg/dL), and close follow-up. And here’s something you won’t hear often: more people are surviving cancer. But that means more people are living with both heart disease and cancer. That’s where cardio-oncology comes in. Cancer treatments like chemotherapy can damage the heart. So now, specialists work together to protect your heart while treating your cancer.
What Happens If You Do Nothing?
Left untreated, atherosclerosis doesn’t just cause heart attacks. It leads to heart failure, irregular heart rhythms, kidney damage, and stroke. The economic cost? In the U.S. alone, heart disease will cost over $1.1 trillion by 2035. But the human cost is worse. You don’t need to be perfect. You don’t need to run marathons. But if you’re over 40, have high blood pressure, smoke, or carry extra weight around your middle-you owe it to yourself to get checked. Even small changes-walking 30 minutes a day, cutting out sugary drinks, quitting smoking-can cut your risk in half.Final Thought: It’s Never Too Late
I’ve seen patients in their 70s, after a heart attack, turn their lives around. One man in Bristol, 76, quit smoking, started walking daily, and dropped his LDL from 140 to 48 in a year. He’s hiking in the Cotswolds now. He didn’t need a miracle. He just started. Coronary artery disease isn’t a death sentence. It’s a warning. And warnings are meant to be heeded.Can you reverse coronary artery disease?
You can’t fully erase plaque, but you can stabilize it and even shrink it slightly. Aggressive lifestyle changes-like a plant-based diet, daily exercise, and strict cholesterol control with statins-have been shown to reduce plaque volume in studies. The goal isn’t perfection. It’s preventing rupture and keeping blood flowing.
Is coronary artery disease the same as heart disease?
Coronary artery disease is the most common type of heart disease. But "heart disease" is a broad term that includes heart failure, arrhythmias, and valve problems. CAD specifically refers to blocked arteries feeding the heart muscle. If you have CAD, you have heart disease. But not all heart disease is CAD.
Do I need a stent if I have chest pain?
Not necessarily. If your chest pain is stable and your heart function is normal, medications and lifestyle changes are just as effective as stents at preventing heart attacks. Stents are best for emergencies-like during a heart attack-or if medications aren’t controlling your symptoms. They don’t make you live longer unless you’re in acute danger.
How often should I get my heart checked?
If you’re over 40 and have risk factors like high blood pressure, diabetes, or smoking, get checked every year. That includes blood pressure, cholesterol, and blood sugar tests. If you’re healthy with no risk factors, start screening at 45-50. Don’t wait for symptoms. By then, it’s often too late.
Can stress cause coronary artery disease?
Chronic stress doesn’t directly cause plaque buildup, but it raises blood pressure, increases inflammation, and leads to unhealthy habits-like overeating, smoking, or skipping exercise. These are the real drivers. Managing stress through sleep, mindfulness, or physical activity helps protect your heart indirectly.
Are natural supplements like fish oil or garlic effective?
Fish oil may help lower triglycerides slightly, but it doesn’t reduce heart attacks in people already taking statins. Garlic, green tea, and other supplements have no strong evidence for preventing or reversing CAD. Don’t replace proven treatments with unproven ones. Focus on food first: fatty fish, nuts, vegetables, and whole grains.
What’s the target LDL cholesterol for someone with CAD?
For people with coronary artery disease, the goal is LDL below 55 mg/dL. That’s much lower than the general population’s target of under 100. Achieving this often requires high-dose statins, sometimes combined with newer drugs like ezetimibe or PCSK9 inhibitors. Don’t settle for "normal"-aim for optimal.

Michaux Hyatt
December 10, 2025 AT 21:36Really great breakdown-especially the part about unstable plaques being the real killers. I’ve seen too many people panic over a 40% blockage and ignore the ones at 30% that blow up out of nowhere. Lifestyle changes are the real MVP here. No pill beats quitting sugar and walking daily.
Raj Rsvpraj
December 11, 2025 AT 13:45India has lower CAD rates than the U.S.-despite eating more carbs!-because we don’t eat processed junk! Your Western diet is the problem, not genetics! Also, statins? Too many side effects! We’ve been using turmeric and neem for centuries!
Jack Appleby
December 12, 2025 AT 00:56Let’s be precise: atherosclerosis isn’t merely "fatty deposits." It’s a chronic, immune-mediated, endothelial dysfunction cascade, driven by oxidized LDL particles infiltrating the intima, triggering macrophage recruitment, foam cell formation, and eventual calcification. The term "plaque" is reductive. And yes-statins reduce LDL by up to 50%, but only if compliant. Non-adherence is the real epidemic.
Also, SGLT2 inhibitors? Brilliant. They’re not just antidiabetics-they’re cardioprotective pleiotropic agents with proven mortality reduction in non-diabetics. The 2023 AHA guidelines were overdue.
Frank Nouwens
December 12, 2025 AT 01:25Thank you for this thoughtful, well-researched post. It’s refreshing to see science communicated without sensationalism. I’ve worked in cardiology for 22 years, and I still find myself sharing this with patients who think a stent is a cure. It’s not. It’s a bandage. The real work is daily.
Kaitlynn nail
December 12, 2025 AT 08:56Plaques are just society’s way of saying "you’re not moving enough."
Aileen Ferris
December 14, 2025 AT 00:03stents are a scam. the real cause is glyphosate in the water. i read it on a blog. also, why do all the docs wear suits? they’re hiding something.
Rebecca Dong
December 14, 2025 AT 09:05THEY DON’T WANT YOU TO KNOW THIS BUT-statins are made by Big Pharma to keep you dependent! They’re poisoning your liver and making you forget your own name! I know a guy who reversed his CAD by eating only raw kale and chanting Tibetan mantras. He’s 89 now. No meds. No stents. Just vibes.
Also-why is the FDA still letting them put sugar in "heart-healthy" cereal? WHO IS CONTROLLING THE SYSTEM??
Michelle Edwards
December 16, 2025 AT 02:49I love how you emphasized that it’s never too late. My mom started walking after her bypass at 72. Now she gardens every morning. She didn’t need to be perfect-just consistent. If you’re reading this and feeling overwhelmed? Start with one walk. One day. That’s enough.
Sarah Clifford
December 16, 2025 AT 04:03so like… if i eat a cheeseburger once a week, am i doomed? because i’m not giving up cheese. also why do people act like heart attacks are just a bad habit? they’re scary!
Regan Mears
December 17, 2025 AT 16:25Thank you for the clarity on plaque stability-it’s something most docs gloss over. I’ve had two family members with silent heart attacks because their "normal" stress tests missed the soft plaques. I now push my 60-year-old brother for a calcium scan every year. It’s not paranoia. It’s prevention.
Also-yes, the LDL target of 55 is non-negotiable for CAD. If your doctor says "under 100 is fine," find a new one.
Ben Greening
December 19, 2025 AT 08:55Coronary artery disease remains the leading cause of death globally. The data is unequivocal. Prevention through modifiable risk factors is both cost-effective and life-saving. The medical community must continue prioritizing population-level education alongside individualized care.
Nikki Smellie
December 20, 2025 AT 23:41Did you know the WHO secretly classifies heart disease as a "population control tool"? 😔 They want us to be afraid of cholesterol so we’ll take pills and not reproduce. I’ve been eating butter and bacon since 2018. My ECG? Perfect. They lied about saturated fat. 😡
Neelam Kumari
December 21, 2025 AT 13:52Oh wow, another white-coat lecture. You sound like every doctor who told me "just lose weight" while ignoring my thyroid and sleep apnea. You know what? I’m 45, 200 lbs, and my LDL is 110. I’m not dying because I eat pizza. I’m dying because the system doesn’t care about people like me.
Queenie Chan
December 22, 2025 AT 23:15This is fascinating-especially the part about cardio-oncology. I had a cousin who survived breast cancer, then developed cardiomyopathy from chemo. No one warned her. Why isn’t this standard? We treat cancer like it’s a standalone battle, but the body doesn’t work that way. Shouldn’t every oncologist have a cardiac consult built into the protocol?
Stephanie Maillet
December 24, 2025 AT 19:07There’s a deeper truth here: we treat the artery, not the person. We obsess over LDL numbers, yet ignore loneliness, chronic stress, and spiritual disconnection-all of which elevate cortisol, inflammation, and endothelial damage. The body doesn’t separate mind from vessel. Maybe healing isn’t just about statins… but belonging.
David Palmer
December 24, 2025 AT 20:41so like… if i stop eating bread, does that mean i’m cured? because i hate bread. also why do they call it "coronary"? is it because it’s the crown of death or something? 🤔
Doris Lee
December 26, 2025 AT 20:12Small steps matter. I started with one apple a day. Then I swapped soda for sparkling water. Then I walked after dinner. Two years later, my LDL dropped 60 points. No drugs. No drama. Just showing up.
Brianna Black
December 27, 2025 AT 21:32As someone raised in a family where heart disease claimed three generations, I want to say: this article is a gift. In my culture, we don’t talk about health until someone collapses. Thank you for giving us the language to speak before it’s too late.
Ryan Brady
December 28, 2025 AT 13:01meh. i eat burgers, drink beer, and still run 5K. your science is weak. 😎