When a pharmacist reaches for a generic pill bottle instead of the brand-name one, it’s not just about saving money. It’s about making a clinical decision - one that requires clear, confident communication with the prescriber. In 2025, over 97% of prescriptions filled in the U.S. are for generic drugs, saving the system nearly $409 billion a year. But behind every substitution is a conversation that often doesn’t happen - or happens poorly.
Why Pharmacists Recommend Generics
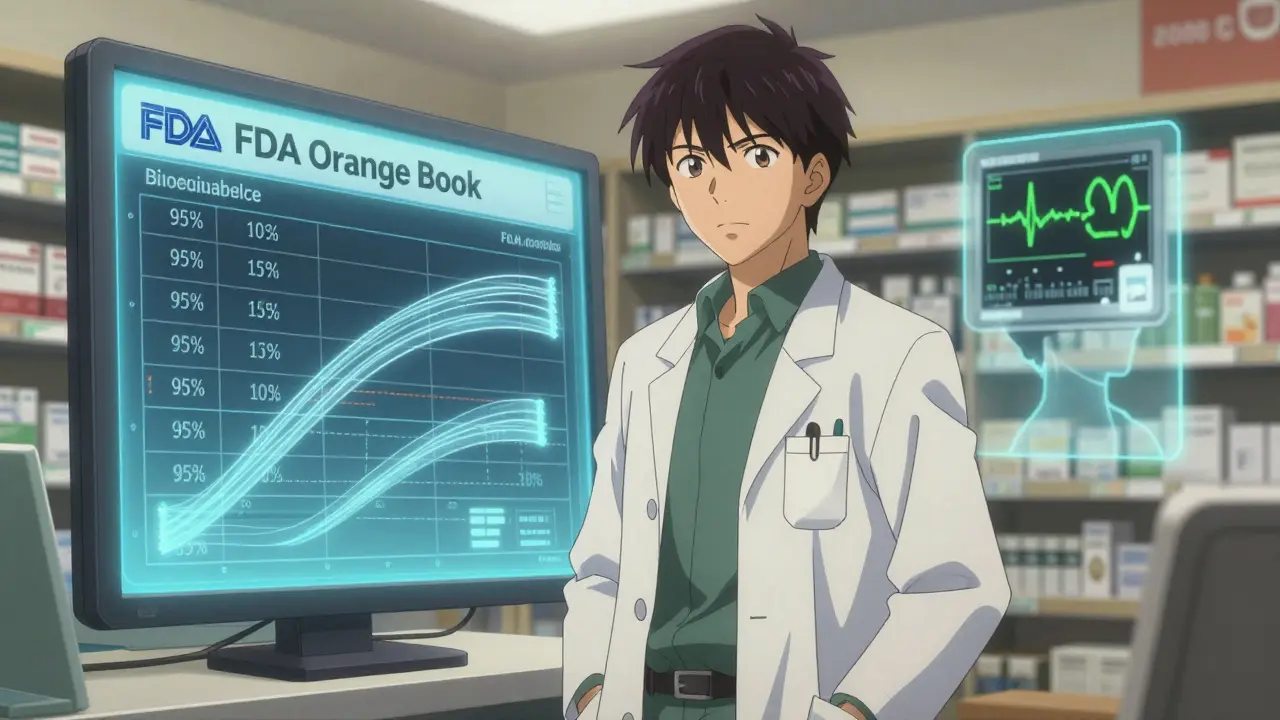
Pharmacists don’t recommend generics because they’re cheaper - though they are. They recommend them because they’re proven to work just as well. The FDA requires generic drugs to meet strict bioequivalence standards: the amount of active ingredient absorbed into the bloodstream must fall within 80% to 125% of the brand-name drug’s levels. Real-world data shows most generics land between 95% and 105%, meaning they’re virtually identical in how the body processes them. A 2018 study tracking 12.7 million patients found people on generics were 12.4% more likely to stick to their medication schedule. That’s not a small win. For someone with high blood pressure or diabetes, missing doses isn’t just inconvenient - it’s dangerous. Better adherence led to a 28.6% drop in non-adherence and a 15.2% reduction in hospital stays. When a pharmacist swaps a brand for a generic and the patient stays healthy and on track, that’s the real success.The Orange Book: The Pharmacist’s Bible
Every pharmacist checking a prescription has one tool they trust more than any other: the FDA’s Orange Book. Officially called Approved Drug Products with Therapeutic Equivalence Evaluations, it’s updated daily and lists every approved generic and its equivalence rating. An "A" rating means the generic is therapeutically equivalent to the brand. A "B" rating means it’s not - and substitution shouldn’t happen. Of the 12,876 generic products listed in the 2023 Orange Book, 92.7% carry an "A" rating. That’s the green light. But pharmacists don’t just flip through pages. They cross-reference the active moiety, dosage form, route of administration, and manufacturer. One wrong step - like substituting a generic with a different salt form - can break therapeutic equivalence. That’s why pharmacists don’t guess. They consult.When Substitution Isn’t Allowed
Not all drugs are safe to swap. The FDA calls these narrow therapeutic index (NTI) drugs. These are medications where even tiny changes in blood levels can cause harm. Think warfarin, levothyroxine, phenytoin, and cyclosporine. For these, the margin between effective and toxic is razor-thin. While the FDA says many generics for NTI drugs are safe, many prescribers still hesitate. Pharmacists know this. When a prescription for levothyroxine comes in, they don’t automatically swap. They check the prescriber’s notes. If it says "dispense as written," they call. They don’t assume. They explain: "This generic has an A rating, and the bioequivalence data shows no clinically significant difference. But if you’ve seen instability in this patient before, I’ll hold off." That kind of conversation builds trust. Another red flag? Excipient allergies. Generics can use different fillers, dyes, or preservatives. One in 12 patients has a documented sensitivity to an inactive ingredient. A patient allergic to lactose? A generic might contain it. A patient with a dye allergy? The brand might use FD&C Red No. 40, but the generic uses tartrazine. Pharmacists flag this. They call the prescriber. They don’t risk a rash - or anaphylaxis - for a $5 savings.
What "Dispense as Written" Really Means
About 15.3% of prescriptions have "DAW" or "dispense as written" written on them. That doesn’t always mean the prescriber distrusts generics. In 68% of cases, it’s because the patient had a bad experience - maybe a switch caused dizziness or a flare-up. Or the prescriber heard an old myth: "Generics aren’t as strong." Pharmacists don’t ignore DAW orders. They respect them. But they also educate. They say: "I see you marked DAW. This patient was switched last year and had no issues. Here’s the bioequivalence data from the Orange Book. The generic we’re considering has the same active ingredient, same release profile, and was used in over 2 million prescriptions last year with no safety alerts. Can we try it?" A 2021 study found that when pharmacists used structured communication - referencing the Orange Book, showing cost savings, and citing real data - prescribers accepted generic recommendations 82.4% of the time. Without structure? Just 57.3%. The difference isn’t luck. It’s preparation.How Communication Is Changing
Gone are the days of scribbling notes on prescription pads and calling the office during lunch. Today, most pharmacies use EHR-integrated tools like Surescripts. A pharmacist can send a secure message directly into the prescriber’s chart. The system auto-populates the generic name, NDC, manufacturer, and even links to the FDA’s Product-Specific Guidance document for that drug. The whole exchange takes 2.7 minutes - down from over 8. And it’s not just about speed. Documentation is now 94.8% complete with digital tools, compared to just 63.5% with paper. That matters. Medicare audits check this. Pharmacies with full records have 98.7% compliance. Those without? They get flagged. They get fined. New tools are emerging, too. AI platforms like PharmAI’s Generic Substitution Assistant analyze patient history, prescriber patterns, and drug databases in seconds. They suggest the best generic, flag potential allergies, and even draft the message to send. Adoption is growing: 28.7% of chain pharmacies use them now. Accuracy jumped from 76.4% to 94.2%.Barriers - And How to Break Them
Still, resistance exists. A 2023 Medscape survey found 58.3% of prescribers worry about generic efficacy. For inhalers, that number hits 42.3%. For topical creams, 38.9%. Why? Because these are complex formulations. The active ingredient is only part of the story. The delivery system - the propellant, the base, the particle size - matters. Pharmacists who succeed don’t say, "It’s the same drug." They say, "This generic uses the same active ingredient and meets the FDA’s Product-Specific Guidance for aerosol delivery. The particle size distribution matches the brand. Here’s the bioequivalence study from the Journal of Pharmaceutical Sciences." Time is another barrier. Pharmacists report only 2.3 minutes per prescription to verify, counsel, and communicate. That’s not enough. But prioritizing high-risk cases - NTI drugs, allergy flags, DAW prescriptions - makes the difference. A pharmacist who calls on just five high-risk cases a day can prevent dozens of medication errors and hospitalizations over a year.

Robyn Hays
December 28, 2025 AT 17:38Okay but have you ever tried switching someone from brand-name levothyroxine to a generic and watched their TSH go haywire for three months? I’ve seen it. Not because the drug is bad - because the patient’s body had already stabilized on that exact formulation. It’s not about generics being inferior, it’s about biological individuality. We treat pills like interchangeable Lego blocks, but human physiology? Not so much.
And don’t get me started on the excipients. One patient had a chronic rash that vanished the moment we switched back to the brand - turned out the generic used a dye she was allergic to. No one asked. No one checked. Just assumed.
Pharmacists aren’t just pharmacists anymore. They’re clinical detectives with access to the Orange Book and a moral compass. We need to stop treating them like cashiers.
Also - why do we still call them ‘generics’? That word makes them sound like knockoffs. They’re bioequivalent therapeutics. Say it like you mean it.
And yes, I’ve emailed my prescriber with FDA links. They usually reply with ‘I’ll think about it.’ That’s not good enough.
Liz MENDOZA
December 29, 2025 AT 22:49I work in a rural clinic and I’ve seen firsthand how cost drives adherence. A patient on warfarin used to skip doses because the brand was $120 a month. Switched to generic - $8. She’s been stable for 14 months. No drama. No hospital visits.
It’s not magic. It’s math. And empathy. The pharmacist who called the doctor? He didn’t just save money. He saved her from a stroke.
Let’s stop acting like generics are a compromise. They’re the default. The brand is the exception. We just haven’t caught up to that reality yet.
Anna Weitz
December 30, 2025 AT 18:07So we’re saying pharmacists are the real gatekeepers of healthcare now and prescribers are just signing forms and hoping for the best
And the Orange Book is the only thing standing between us and a nationwide pharmaceutical chaos
And AI is gonna fix everything but we still don’t know if a generic for an inhaler is actually the same because the propellant is different and nobody tested it in real people
Also why are we still using paper pads in 2025
And why does no one talk about how the FDA approves generics based on lab data not actual human outcomes
And why are we surprised when people get weird side effects after switching
It’s all just a big system built on trust and hope and 2.3 minutes per prescription
And we wonder why people don’t trust medicine
dean du plessis
January 1, 2026 AT 01:31Back home in South Africa we don’t even have this debate. Generics are the only option for most people. The system works because we don’t have the luxury of brand-name delusions. We trust the science, not the marketing.
Here, it’s like we’ve turned medicine into a luxury brand. If it doesn’t have a fancy logo, it’s not real. That’s the real problem.
Pharmacists are doing the work. The rest of us are just arguing about labels.
Kylie Robson
January 1, 2026 AT 04:24Let’s be precise: the FDA’s bioequivalence range of 80–125% is a statistical construct derived from Cmax and AUC parameters under fasting conditions - not reflective of steady-state pharmacokinetics in polypharmacy patients with renal impairment or CYP450 polymorphisms.
When you say ‘virtually identical,’ you’re conflating population-level bioequivalence with individual therapeutic equivalence. That’s a categorical error.
Moreover, the Orange Book’s A-rating does not account for excipient variability across manufacturers, which can alter dissolution profiles in extended-release formulations - particularly problematic with NTI drugs like phenytoin where Cmax variability >15% correlates with seizure recurrence.
And don’t get me started on the lack of post-marketing surveillance for generics. The FDA’s passive adverse event reporting system is statistically underpowered to detect signals in low-incidence, high-severity events.
AI tools? They’re trained on biased datasets. PharmAI’s model was validated on Medicare Part D claims, which exclude Medicaid and uninsured populations - where substitution rates are highest.
So yes, 92.7% of generics are A-rated. But that doesn’t mean they’re clinically interchangeable. The data is incomplete. The science is nuanced. And we’re oversimplifying to the point of dangerous.
Caitlin Foster
January 3, 2026 AT 03:27So let me get this straight - pharmacists are now the brain surgeons of the drug world, doing 2.3-minute consults while juggling 30 prescriptions, calling prescribers like they’re calling tech support, and somehow we’re still surprised when people get confused or sick?
And we’re patting ourselves on the back because we have an AI that can draft a message in 2.7 minutes? That’s not innovation - that’s a band-aid on a broken system!
Meanwhile, doctors are still getting paid to write scripts, not to understand them. And patients? They’re just trying not to die while paying $200 for a pill that’s been around since 1998.
Let’s just rename the whole thing: ‘The Great Generic Confusion™’ - sponsored by Big Pharma and the American Healthcare Indifference Association.
Also - who approved this as a TED Talk?!
Todd Scott
January 5, 2026 AT 01:24As someone who spent five years working in community pharmacy across three states, I can tell you this: the biggest barrier isn’t prescriber resistance or even patient fear - it’s time. And by time, I mean the complete absence of systemic support.
Pharmacists are expected to be clinicians, educators, data analysts, legal documenters, and patient advocates - all while standing behind a counter, answering phones, managing inventory, and dealing with insurance denials. The average pharmacist works 45 hours a week and has 8 minutes per patient for counseling - if they’re lucky.
And yet, when a patient has an adverse reaction after a switch, the blame lands on the pharmacist. Not the system. Not the lack of reimbursement for counseling. Not the fact that EHRs still don’t talk to each other properly.
We need to stop asking pharmacists to do more with less and start asking: why are we paying doctors $400 to write a script and $10 to review it?
Value-based care isn’t about savings. It’s about redefining roles. Pharmacists aren’t just filling bottles - they’re preventing hospitalizations. They’re reducing readmissions. They’re saving lives. And we’re treating them like glorified clerks.
It’s time to pay them like the clinicians they are. Not because it’s fair - because it’s the only way this system survives.
Chris Garcia
January 6, 2026 AT 19:50In Nigeria, we do not have the luxury of brand-name drugs. Everything is generic. And yet, our mortality rates for hypertension and diabetes are higher than in the U.S. Why? Because access is not the same as quality. Because supply chains are broken. Because there is no Orange Book. Because pharmacists are not trained to interpret bioequivalence data. Because no one documents anything.
So I look at your system - your databases, your AI, your secure messaging - and I see a beautiful machine. But I also see a machine that assumes the foundation is solid.
It is not.
The real innovation is not in the technology. It is in the culture. In the respect. In the time. In the trust.
When a pharmacist calls a prescriber and says, ‘I have data. I have concern. I have care,’ that is the revolution.
Not the algorithm.
Not the savings.
But the conversation.