Anticoagulant Dosing Calculator
Dosing Calculator
Enter eGFR (mL/min) to see recommended DOAC doses for kidney disease
Results
eGFR: mL/min
| Anticoagulant | Recommended Dose | Notes |
|---|
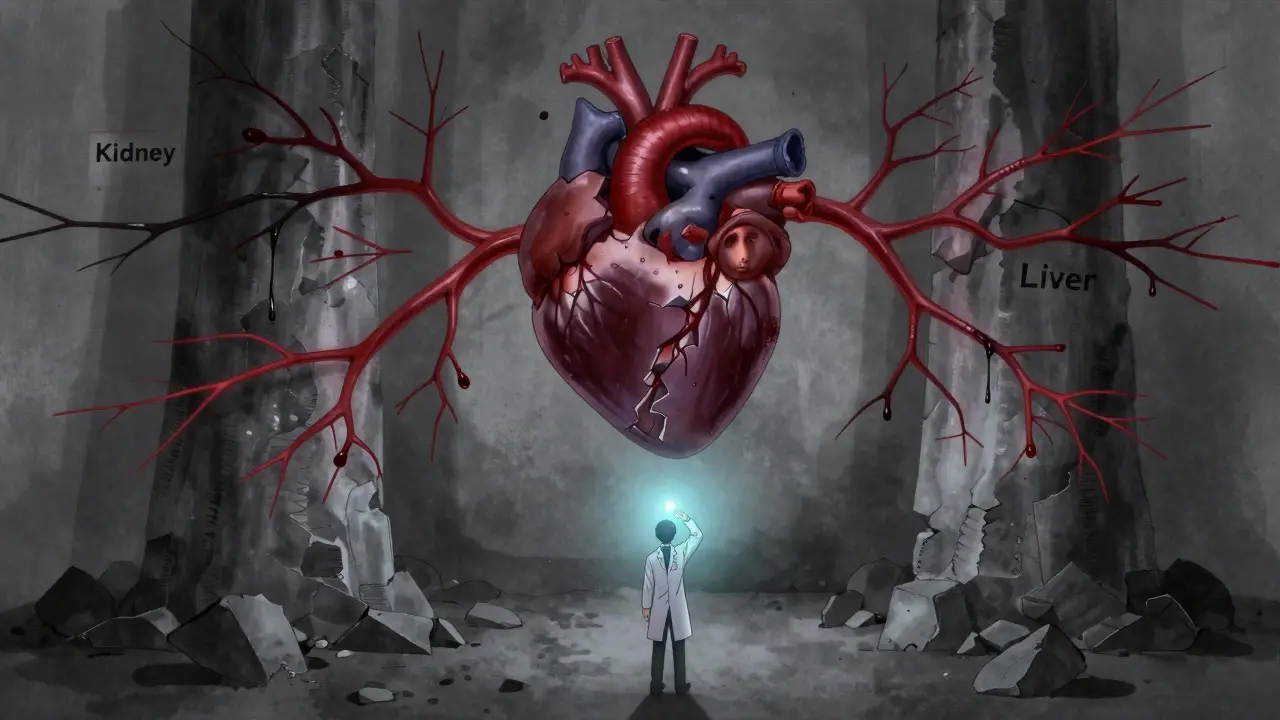
Managing blood thinners in people with both kidney and liver disease isn’t just complicated-it’s risky. These patients are caught between two dangers: clotting that can cause strokes or pulmonary embolisms, and bleeding that can be deadly. Yet, for years, doctors have had to guess because most clinical trials excluded them. Today, we’re breaking down what actually works, what doesn’t, and how real-world experience is changing the rules.
Why Standard Blood Thinners Don’t Work the Same Here
Most anticoagulants were tested on healthy adults. But if you have kidney disease, your body clears drugs differently. If you have liver disease, your body makes fewer clotting factors. These aren’t minor adjustments-they change how dangerous or effective a drug becomes. Take the DOACs: dabigatran, rivaroxaban, apixaban, edoxaban. They were supposed to replace warfarin because they’re easier to use. But in patients with advanced kidney or liver disease, the data is thin. The RE-LY, ROCKET-AF, ARISTOTLE, and ENGAGE AF trials didn’t include people with eGFR below 30 mL/min or Child-Pugh C cirrhosis. That means the labels you see on the bottle? They’re based on guesswork.Kidney Disease: It’s Not Just About eGFR Numbers
Doctors often rely on eGFR to judge kidney function. But in advanced kidney disease, creatinine-based estimates like CKD-EPI can be off by 30-40%. A number might look stable, but your kidneys could be failing fast. That’s why monitoring trends matters more than single values. For early kidney disease (eGFR ≥45 mL/min), all DOACs are generally safe. But once you hit stage 3b (eGFR 30-44), dose changes kick in:- Apixaban drops from 5 mg to 2.5 mg twice daily
- Rivaroxaban drops from 20 mg to 15 mg daily
- Edoxaban drops from 60 mg to 30 mg daily
Liver Disease: The INR Lie
The INR is the gold standard for warfarin monitoring. But in liver disease? It’s a lie. In cirrhosis, your liver doesn’t make enough clotting factors. But it also doesn’t make enough natural anticoagulants like protein C and S. Your platelets drop too-76% of cirrhotic patients have counts under 150,000/μL. So your INR might look high, but you’re not necessarily at higher risk of bleeding. Or worse, it might look normal, but you’re about to hemorrhage. The Child-Pugh score is the best way to stratify risk:- Child-Pugh A (score 5-6): DOACs are generally okay at standard doses
- Child-Pugh B (score 7-9): Use with caution; consider dose reduction
- Child-Pugh C (score ≥10): DOACs are contraindicated

DOACs vs. Warfarin: The Real Numbers
Let’s cut through the noise with hard data:- In CKD stages 3-4, apixaban cuts major bleeding by 31% compared to warfarin
- Dabigatran is cleared 80% by the kidneys-so it’s off the table at eGFR <30
- Apixaban is cleared only 27% by kidneys, making it the most forgiving DOAC in kidney disease
- DOACs reduce intracranial hemorrhage by 62% in CKD patients compared to warfarin
- In end-stage renal disease (ESRD), warfarin may still be preferred for mechanical heart valves
Real-World Chaos: What Happens in the Clinic
A 2021 registry of 12,850 dialysis patients with atrial fibrillation found only 28.4% were on anticoagulation-even though 76% had high stroke risk (CHA2DS2-VASc ≥3). Of those treated:- 63% got warfarin
- 37% got DOACs

What’s Coming Next
Two major trials are underway. The MYD88 trial is randomizing 500 dialysis patients to apixaban versus warfarin. Results are due in 2025. The LIVER-DOAC registry is tracking 1,200 cirrhotic patients on DOACs worldwide. The FDA is drafting new labeling for apixaban in ESRD. KDIGO plans to update its guidelines in late 2024, incorporating 17 new observational studies. Until then, the best advice is simple: don’t treat the number. Treat the person.- Check kidney function monthly if eGFR is dropping
- Check platelets and MELD score monthly in liver disease
- Never assume a DOAC is safe just because it’s labeled “for kidney disease”
- When in doubt, consult nephrology and hepatology together
Reversal Is Rarely Ready
If a patient bleeds, can you reverse it? Probably not quickly. Andexanet alfa reverses apixaban and rivaroxaban-but it’s expensive and only available in 45% of U.S. hospitals. Idarucizumab reverses dabigatran-but costs $3,500 and does nothing for other DOACs. Warfarin? You can give vitamin K and plasma. But it takes hours to work. And here’s the kicker: 78% of U.S. hospitals have no formal protocol for managing anticoagulation in patients with both kidney and liver disease. That’s why medication errors are 3.2 times more common in this group.Bottom Line
There’s no perfect answer. But here’s what works today:- For kidney disease: Apixaban is the safest DOAC, even in advanced stages
- For liver disease: Avoid DOACs if Child-Pugh C. Use warfarin only if you can monitor closely
- For both: Avoid dabigatran. It’s too dependent on kidney function
- For dialysis: Consider apixaban 2.5 mg twice daily-but only after careful risk review
- Always involve specialists. One doctor can’t manage this alone
Can I take apixaban if I’m on dialysis?
Yes, but only at a reduced dose: 2.5 mg twice daily. This is based on pharmacokinetic data and post-hoc analysis from the ARISTOTLE trial. However, there’s no large randomized trial proving it prevents strokes in dialysis patients. Many doctors use it because it has the lowest bleeding risk among DOACs in kidney disease, but it’s not FDA-approved for this use. Always discuss with your nephrologist and cardiologist.
Is warfarin safer than DOACs in liver disease?
It depends. Warfarin has better reversal options and is cheaper, but it’s harder to keep in range in cirrhosis. INR becomes unreliable because your liver can’t make clotting factors consistently. DOACs are safer for stroke prevention, but if you have Child-Pugh C cirrhosis, they’re not safe at all. For Child-Pugh A or B, DOACs may be better-but only if you have access to monitoring tools like TEG or ROTEM. Most clinics don’t, so warfarin remains common despite its challenges.
Why is dabigatran not recommended in kidney disease?
Dabigatran is cleared 80% by the kidneys. In advanced kidney disease (eGFR <30 mL/min), it builds up in the blood, increasing bleeding risk. That’s why it’s contraindicated at eGFR below 30. Even in moderate kidney disease, it’s riskier than apixaban or edoxaban. Apixaban, by contrast, is only 27% cleared by the kidneys, making it much safer in this group.
Can I switch from warfarin to a DOAC if I have both kidney and liver disease?
It’s possible-but risky. If your kidney function is stage 3b or worse and your liver disease is Child-Pugh B or C, switching to a DOAC is not recommended. The data doesn’t support it. If you’re stable on warfarin with good INR control, staying on it may be safer. If you’re struggling to keep INR in range, a DOAC might help-but only if your organ function is mild (eGFR >45, Child-Pugh A). Always get input from both a hematologist and hepatologist before switching.
What tests should I have if I’m on blood thinners with kidney or liver disease?
For kidney disease: eGFR every 3 months (monthly if declining). For liver disease: platelet count and MELD score every month. If you’re on warfarin, INR should be checked every 2-4 weeks. If you’re on a DOAC, no routine lab tests are needed-but if you’re at high risk of bleeding, ask about TEG or ROTEM. Also, track for signs of bleeding: bruising, dark stools, headaches, or abdominal pain. Don’t wait for a lab result to act.