Most people think of painkillers like ibuprofen or acetaminophen as harmless, everyday tools-something you grab from the cabinet when your head hurts or your back flares up. But what if taking a few pills a day for years was slowly damaging your kidneys? That’s exactly what analgesic nephropathy is: a silent, preventable form of kidney damage caused by long-term, high-dose use of common pain medications. It doesn’t come with warning signs until it’s too late. By then, the damage is often permanent.
How Painkillers Turn Into Kidney Killers
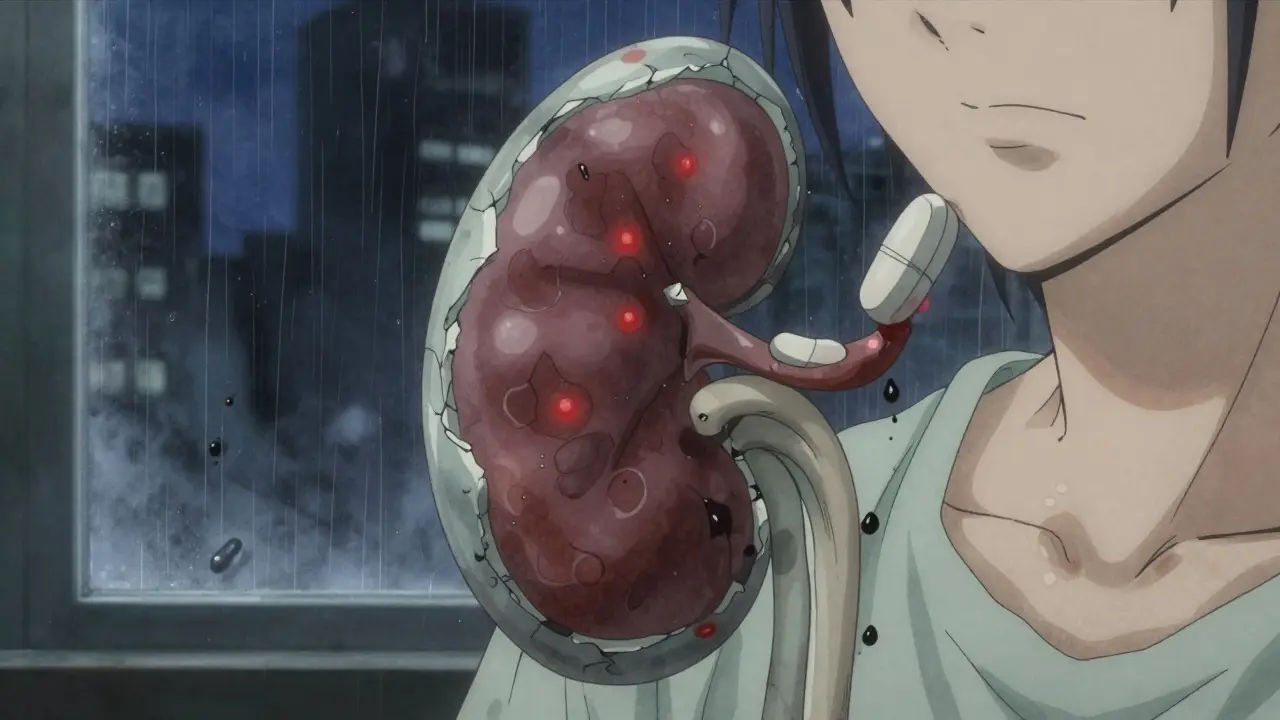
Your kidneys don’t just filter waste-they regulate blood pressure, balance fluids, and keep your body’s chemistry stable. When you take NSAIDs like ibuprofen, naproxen, or aspirin regularly, they block chemicals called prostaglandins that help keep blood flowing to your kidneys. Less blood flow means less oxygen, which stresses kidney tissue. Over time, this leads to scarring in the inner parts of the kidney, especially around the renal papillae-the tiny structures that collect urine.
This isn’t just theory. Studies show that people who take six or more pain pills daily for three years or more have a dramatically higher risk. The damage starts quietly: no pain, no swelling, no symptoms. The only clue? A slight rise in creatinine levels during a routine blood test. By the time someone feels tired, puffy, or notices blood in their urine, the kidneys are already struggling.
Historically, phenacetin-a now-banned ingredient in combo painkillers like Excedrin and Anacin-was the biggest culprit. In Australia during the 1970s and 80s, it caused up to 10% of all end-stage kidney disease cases. Even after phenacetin was pulled from shelves, NSAIDs kept the problem alive. Today, it’s not the old combo pills-it’s the daily ibuprofen for arthritis, the nightly Excedrin for migraines, the naproxen for back pain that’s quietly doing the damage.
Who’s Most at Risk?
This isn’t just an old person’s problem. The highest risk group? Women between 35 and 55. Why? Many are managing chronic headaches, menstrual pain, or arthritis-and they’ve been told for decades that OTC painkillers are safe. A 2021 study found that 72% of analgesic nephropathy cases occur in women. They’re not overdoing it out of recklessness; they’re trying to live normally.
Other high-risk groups include people with existing high blood pressure, diabetes, or early kidney disease. Even if your kidneys seem fine now, NSAIDs can accelerate decline. The National Kidney Foundation warns that daily NSAID use beyond 10 days should be avoided without medical supervision. Yet, a 2023 CDC report found that 41% of U.S. adults exceed recommended doses-especially those with chronic pain.
And here’s the kicker: acetaminophen isn’t a safe alternative if you’re taking it too much. While it’s less harmful to kidneys than NSAIDs, daily use over 4,000 mg for five years increases chronic kidney disease risk by 68%, according to a 2020 study in Kidney International Reports. That’s two extra-strength Tylenol tablets, four times a day-every day-for years. Many people don’t realize they’re hitting that limit.
The Silent Progression: From No Symptoms to Dialysis
Analgesic nephropathy doesn’t hit like a heart attack. It creeps in.
- Years 1-3: No symptoms. Kidney function appears normal on routine labs.
- Years 4-7: Slight rise in creatinine. Blood pressure starts climbing. Urine tests show tiny amounts of protein or white blood cells (sterile pyuria).
- Years 8+: Fatigue, swelling in ankles, frequent urination at night. Anemia develops because kidneys stop making erythropoietin.
- Advanced stage: Flank pain, blood in urine, even passing pieces of dead kidney tissue (papillae). At this point, GFR (kidney filter rate) may drop below 45-signaling moderate to severe damage.
One patient on Reddit, who went by ‘ChronicPainWarrior99,’ shared: “I took 8-10 Excedrin Migraine tablets daily for 7 years before my GFR dropped to 45. My nephrologist said I was lucky it wasn’t worse-many people need dialysis from this.”
That’s the turning point. Once the kidneys are scarred, you can’t reverse it. But you can stop it from getting worse-if you catch it early.
How Doctors Diagnose It
There’s no single test for analgesic nephropathy. Diagnosis is a puzzle:
- Blood tests: Rising creatinine and falling eGFR signal kidney trouble.
- Urine tests: Bland sediment (no red blood cells or casts) and non-nephrotic proteinuria (less than 3.5 g/day) are classic signs.
- Imaging: A noncontrast CT scan can show calcified renal papillae-a hallmark of advanced damage. It’s 87% sensitive and 97% specific.
- History: The biggest clue? A long history of daily painkiller use, especially combination products with caffeine or codeine.
And now, there’s a new tool: NephroCheck, a point-of-care urine test approved by the FDA in January 2023. It detects early signs of papillary damage with 92% accuracy-before creatinine even starts to climb. This could be a game-changer for high-risk patients.
What Happens If You Stop?
Here’s the good news: stopping the painkillers can save your kidneys.
A 2022 study in the Clinical Journal of the American Society of Nephrology followed 142 patients who stopped NSAIDs and acetaminophen after early diagnosis. After five years, 73% had stable kidney function. None got worse. That’s not a cure-but it’s a halt. And for many, it’s enough to avoid dialysis.
But quitting painkillers isn’t easy. On PatientsLikeMe, 41% of users said they struggled to manage pain after stopping NSAIDs. Many felt abandoned by their doctors. “They took away my pills but didn’t give me anything else,” one wrote.
Safer Ways to Manage Chronic Pain
You don’t have to suffer. There are effective, kidney-safe alternatives.
- Topical NSAIDs: Gels and patches like diclofenac gel deliver pain relief directly to the joint with 90% less systemic absorption. A 2021 trial showed they work just as well as oral pills for osteoarthritis-with zero impact on kidney function.
- Heat therapy: Devices like ThermaCare HeatWraps reduce osteoarthritis pain by 40-60%. No chemicals. No risk. FDA-cleared since 2022.
- Physical therapy: The American College of Rheumatology recommends trying PT for 4-6 weeks before even touching a pill. Strengthening muscles around joints reduces strain and pain.
- Cognitive behavioral therapy (CBT): Chronic pain changes your brain. CBT helps rewire how you respond to pain, reducing reliance on meds. Proven effective for migraines, back pain, and fibromyalgia.
- Prescription alternatives: For migraines, CGRP inhibitors (like Aimovig or Emgality) work without touching the kidneys-but they cost $650/month. For some, the trade-off is worth it.
And if you must use oral meds? Stick to the limits:
- NSAIDs: No more than 1,200 mg ibuprofen or 750 mg naproxen per day for chronic use.
- Acetaminophen: Never exceed 3,000 mg per day (that’s six 500 mg tablets).
- Frequency: No more than three days a week without talking to your doctor.

The Bigger Picture: Why This Matters
Analgesic nephropathy isn’t rare. In the U.S., it causes 15,000-20,000 new cases of chronic kidney disease every year. That’s 2-3% of all CKD cases. The cost? $18,500 per patient annually for early care. If it progresses to dialysis? $90,000 per year.
And it’s entirely preventable. The Mayo Clinic’s Chief of Nephrology says up to 70% of cases could be avoided with better education and monitoring. The FDA updated NSAID labels in 2020 to include kidney risk warnings. Companies like Bayer and Johnson & Johnson have reformulated products to reduce acetaminophen and remove caffeine.
But awareness is still low. A Cedars-Sinai survey found 62% of patients didn’t believe OTC painkillers could harm their kidneys. That’s the real problem-not the pills themselves, but the myth that they’re harmless.
What You Can Do Today
Here’s your action plan:
- Check your medicine cabinet. Count how many pills you take per week. Are they NSAIDs? Acetaminophen? Combo packs?
- If you’re taking more than three days a week, talk to your doctor. Ask: “Could this be hurting my kidneys?”
- Get a simple blood test: creatinine and eGFR. It’s cheap, fast, and tells you more than you think.
- Try one non-drug option this week: a heating pad, a 20-minute walk, or a breathing exercise.
- Write down your pain triggers. What makes it worse? What helps? That’s data your doctor can use to find safer solutions.
You don’t have to live in pain. But you also don’t have to sacrifice your kidneys to feel better. The right balance exists. It just takes awareness-and a willingness to ask the hard questions.
Can taking ibuprofen every day cause kidney damage?
Yes. Daily use of ibuprofen-even at over-the-counter doses-can reduce blood flow to the kidneys and cause scarring over time. The risk increases significantly if you take more than 1,200 mg per day for over three years. People with high blood pressure, diabetes, or existing kidney disease are at highest risk.
Is acetaminophen safer for kidneys than NSAIDs?
Acetaminophen is generally less harmful to kidneys than NSAIDs, but it’s not risk-free. Taking more than 3,000 mg daily for five years increases the risk of chronic kidney disease by 68%, according to a 2020 study. The danger comes from long-term, high-dose use-not occasional use.
Can analgesic nephropathy be reversed?
Once scarring occurs, it can’t be undone. But stopping the painkillers can stop further damage. Studies show that 73% of patients who quit NSAIDs and acetaminophen early saw their kidney function stabilize and never decline again. Early detection is key.
What are the first signs of kidney damage from painkillers?
There often are no early signs. The first clue is usually a routine blood test showing rising creatinine or a drop in eGFR. Later symptoms include fatigue, swelling in legs, increased nighttime urination, and high blood pressure. By the time you feel unwell, damage is already advanced.
What’s the best pain relief option if I have kidney problems?
Topical NSAID gels (like diclofenac) are the safest oral alternative-they deliver pain relief with minimal kidney exposure. Heat therapy, physical therapy, and CBT are non-drug options with strong evidence. Always avoid combination painkillers with caffeine or codeine. Talk to your doctor about your specific condition before choosing any treatment.
How often should I get my kidneys checked if I take painkillers regularly?
If you take NSAIDs or acetaminophen daily for more than 10 days a month, get a blood test (creatinine and eGFR) every 6 months. If you have high blood pressure, diabetes, or a history of kidney issues, get tested every 3 months during the first 6 months of use. Early detection saves kidneys.
What Comes Next?
The future of pain management is shifting. Researchers are developing new drugs that relieve pain without affecting kidney blood flow. AstraZeneca’s selepressin, for example, showed promise in reducing NSAID-induced kidney stress in Phase II trials. The American Society of Nephrology has allocated $12 million to develop “kidney-sparing analgesics.”
But innovation won’t help if people don’t change their habits. The real breakthrough will come when patients stop seeing painkillers as harmless and start seeing them as medicine-with risks, limits, and alternatives.
Don’t wait for a blood test to tell you something’s wrong. Ask questions. Try something new. Protect your kidneys the same way you protect your heart or your liver. Because once they’re damaged, you can’t just take a pill to fix them.


Juan Reibelo
January 23, 2026 AT 23:48I used to take ibuprofen like candy-two after work, two after gym, two before bed. Then my doc said my creatinine was creeping up. I thought he was being dramatic. Turns out, he was just being a doctor. I switched to heat wraps and PT. My kidneys are stable now. No more pills. No more guilt.
Vatsal Patel
January 24, 2026 AT 16:43Oh wow, so now we’re supposed to feel bad for taking Tylenol? Let me guess-the FDA will next ban breathing because it might cause lung damage if done too much. Meanwhile, in India, people take 10 pills a day for decades and still run marathons. Maybe the real problem is overmedicating your anxiety with medical jargon?
blackbelt security
January 26, 2026 AT 11:48This is the wake-up call we all need. Stop treating painkillers like candy. Your kidneys don’t scream-they whisper. And by the time you hear them? It’s too late. Start small. One day without pills. Try a heating pad. Walk 10 minutes. Your future self will thank you.
Patrick Gornik
January 27, 2026 AT 10:29Let’s be real-this isn’t about kidneys. It’s about the pharmaceutical-industrial complex’s need to sell you a problem so they can sell you a solution. You think your doctor cares about your renal papillae? Nah. They care about your insurance copay. Topical NSAIDs? Sure. But they’re 10x more expensive. Meanwhile, your grandma in rural Texas takes aspirin like Tic Tacs and lives to 98. Coincidence? Or is the science just… convenient?
Tommy Sandri
January 29, 2026 AT 01:54The clinical evidence presented in this article is both comprehensive and compelling. The epidemiological data regarding long-term analgesic use and its association with chronic kidney disease aligns with peer-reviewed literature from the Journal of the American Society of Nephrology. It is imperative that public health messaging evolve to reflect these findings, particularly among populations with high OTC analgesic consumption.
Luke Davidson
January 30, 2026 AT 04:36I used to think my nightly Excedrin was just part of my routine-like brushing my teeth. Then I found out I was hitting 4000mg a week. I felt like a fool. But I didn’t give up on feeling better-I just switched. Heat pack every night, yoga on weekends, and I started journaling my pain triggers. No more pills. No more fear. Just me, my body, and a whole lot more peace. You can do this too. Seriously.
Karen Conlin
January 31, 2026 AT 06:01Women are the silent victims of this. We’re told to push through pain-menstrual cramps, migraines, backaches-and we do. We take the pills. We don’t complain. We just keep going. But here’s the truth: your body isn’t a machine you can keep running on fumes. Stop. Pause. Ask for help. Try CBT. Try PT. Try heat. You don’t need a pill to be strong. You just need to listen.
asa MNG
January 31, 2026 AT 11:57OMG I JUST REALIZED I’VE BEEN TAKING 8 EXCEDRIN A WEEK FOR 5 YEARS 😱 I THOUGHT IT WAS JUST COFFEE AND ASPIRIN BUT NOW I’M SCARED TO DEATH 💀 I’M GOING TO CRY AND THEN I’M GOING TO CALL MY DOCTOR 🤕😭 #kidneyawareness
Sushrita Chakraborty
February 1, 2026 AT 04:00It is important to note that the prevalence of analgesic nephropathy in developing nations remains underreported due to limited access to diagnostic tools. In India, where OTC analgesics are often consumed without medical supervision, the true burden may be significantly higher than global estimates suggest. Public education campaigns, in local languages, are urgently needed.
Sawyer Vitela
February 1, 2026 AT 21:4173% stabilized? That’s not a win. That’s just not dying faster. You’re still damaged. You’re still one infection away from dialysis. This isn’t prevention. It’s damage control. And it’s too late for most.
Tiffany Wagner
February 3, 2026 AT 17:16I never knew NSAIDs could do this. I’ve been taking naproxen for my arthritis since college. I’m going to switch to the gel tomorrow. And I’ll start walking. Just… one day at a time.
Viola Li
February 4, 2026 AT 19:36They say ‘don’t take NSAIDs daily’ but they don’t say what to do instead. So you suffer. Or you lie to your doctor. Or you keep taking them. This article gives options-but only if you’re wealthy enough to afford PT or CGRP inhibitors. What about the rest of us?
Dolores Rider
February 5, 2026 AT 00:14Did you know the FDA knew about this since the 90s? They buried it. Big Pharma owns the labels. I saw a leaked memo once. They were worried people would stop buying combo pills. So they downplayed the kidney risk. You think your doctor’s giving you advice? Nah. They’re reading the script.
Darren Links
February 6, 2026 AT 06:03My dad had analgesic nephropathy. He took 10 Advil a day for 15 years. He didn’t know. We didn’t know. He ended up on dialysis at 58. This isn’t theoretical. This is real. If you take painkillers daily, get your kidneys checked. It takes five minutes. It could save your life.
Kevin Waters
February 8, 2026 AT 03:27One of my patients stopped all NSAIDs cold turkey and started doing tai chi every morning. Six months later, her eGFR went up 8 points. She said it wasn’t the exercise-it was the peace. She finally stopped fighting her pain and started listening to it. Sometimes the best medicine isn’t in a bottle. It’s in the quiet.